J Adv Prosthodont.
2018 Feb;10(1):18-24. 10.4047/jap.2018.10.1.18.
Survival rate of modern all-ceramic FPDs during an observation period from 2011 to 2016
- Affiliations
-
- 1Department of Prosthetic Dentistry, Biomedical Materials Research, Hannover Medical School, Hannover, Germany. Pott.Philipp-Cornelius@mh-hannover.de
- KMID: 2403994
- DOI: http://doi.org/10.4047/jap.2018.10.1.18
Abstract
- PURPOSE
In literature, many studies compare survival rates of different types of FPDs. Most of them compared restorations, which originated from one university, but from different clinicians. Data about restoration survival rates by only one experienced dentist are very rare. The aim of this study was to evaluate the survival rate of allceramic FPDs without the blurring effects of different clinicians.
MATERIALS AND METHODS
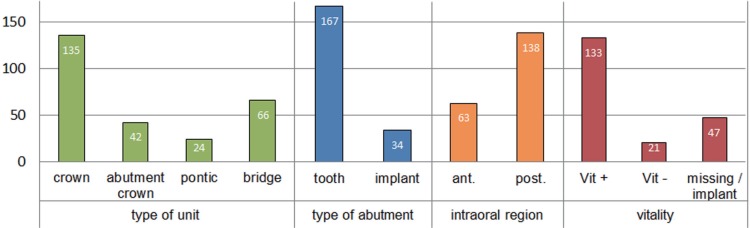
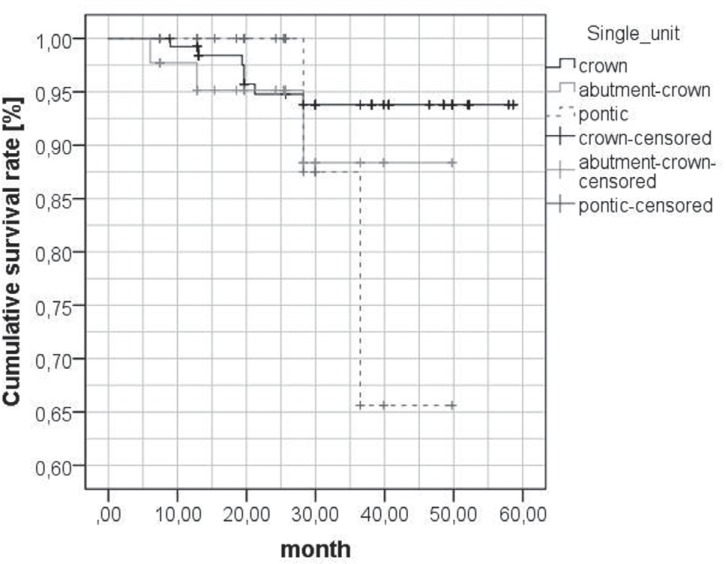
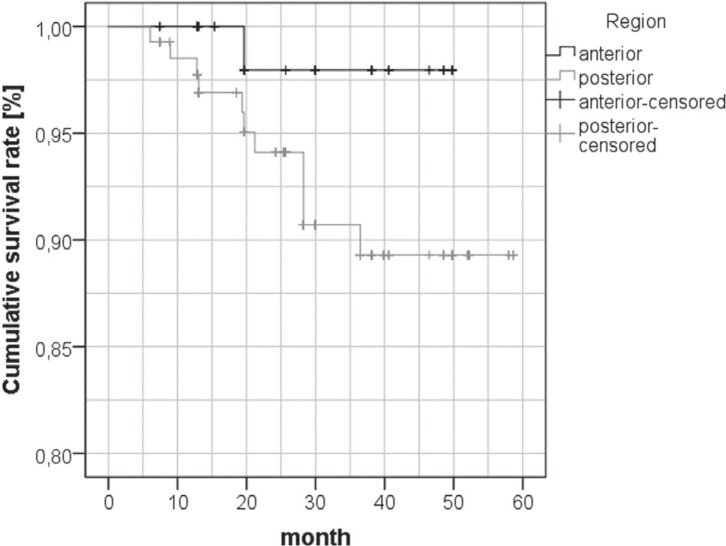
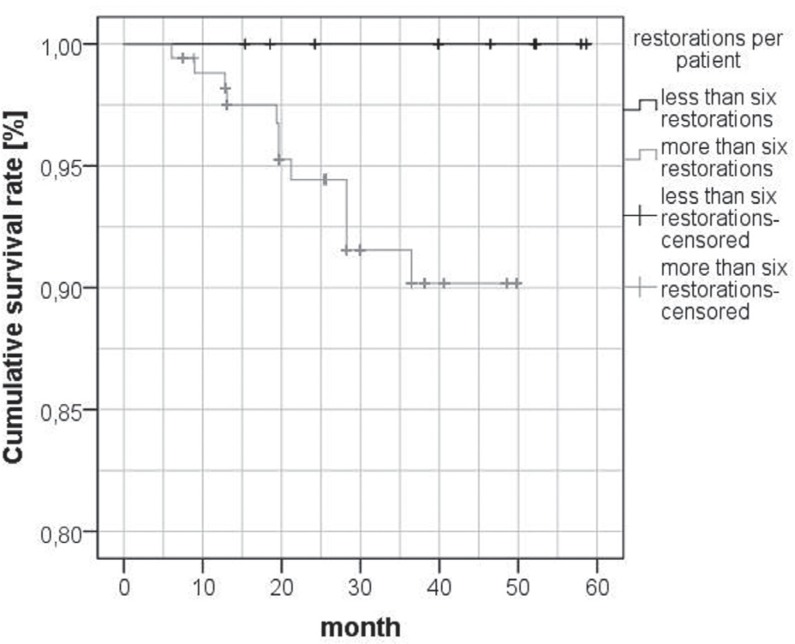
153 veneeredzirconia FPDs were observed for follow-up. 22 patients received 131 single crowns and 22 bridges. Because of the different bridge lengths, one unit was defined as a restored or replaced tooth. In total, 201 units were included. Only the restorations performed by the same clinician and produced in the same dental laboratory from 2011 to 2016 were included. Considered factors were defined as "type of unit", "type of abutment", "intraoral region", and "vitality". Modified UHPHS criteria were used for evaluation. Statistical analysis was performed using cox-regression.
RESULTS
189 units (94.0%) showed no kind of failure. 5 chippings (2.4%) could be corrected by intraoral polishing. 4 units (1.9%) exhibited spontaneous decementation. These polishable and recementable restorations are still in clinical use. Chippings or decementations, which lead to total failure, did not occur. One unit was completely fractured (0.5 %). Biological failures (caries, periodontitis or periimplantitis) did not occur. The statistical analysis of the factors did not reveal any significant differences.
CONCLUSION
Modern all-ceramic FPDs seem to be an appropriate therapy not only for single restorations but for complex occlusal rehabilitations.
Keyword
MeSH Terms
Figure
Reference
-
1. Schmitter M, Mueller D, Rues S. Chipping behaviour of allceramic crowns with zirconia framework and CAD/CAM manufactured veneer. J Dent. 2012; 40:154–162. PMID: 22197634.
Article2. Alhasanyah A, Vaidyanathan TK, Flinton RJ. Effect of core thickness differences on post-fatigue indentation fracture resistance of veneered zirconia crowns. J Prosthodont. 2013; 22:383–390. PMID: 23387466.
Article3. Molin MK, Karlsson SL. Five-year clinical prospective evaluation of zirconia-based Denzir 3-unit FPDs. Int J Prosthodont. 2008; 21:223–227. PMID: 18548960.4. Naenni N, Bindl A, Sax C, Hämmerle C, Sailer I. A randomized controlled clinical trial of 3-unit posterior zirconia-ceramic fixed dental prostheses (FDP) with layered or pressed veneering ceramics: 3-year results. J Dent. 2015; 43:1365–1370. PMID: 26234623.
Article5. Ramos GF, Monteiro EB, Bottino MA, Zhang Y, Marques de Melo R. Failure probability of three designs of zirconia crowns. Int J Periodontics Restorative Dent. 2015; 35:843–849. PMID: 26509988.
Article6. Harianawala HH, Kheur MG, Apte SK, Kale BB, Sethi TS, Kheur SM. Comparative analysis of transmittance for different types of commercially available zirconia and lithium disilicate materials. J Adv Prosthodont. 2014; 6:456–461. PMID: 25551005.
Article7. Kohorst P, Borchers L, Strempel J, Stiesch M, Hassel T, Bach FW, Hübsch C. Low-temperature degradation of different zirconia ceramics for dental applications. Acta Biomater. 2012; 8:1213–1220. PMID: 22138551.
Article8. Marquardt P, Strub JR. Survival rates of IPS empress 2 all-ceramic crowns and fixed partial dentures: results of a 5-year prospective clinical study. Quintessence Int. 2006; 37:253–259. PMID: 16594356.9. Moráguez OD, Wiskott HW, Scherrer SS. Three- to nine-year survival estimates and fracture mechanisms of zirconia- and alumina-based restorations using standardized criteria to distinguish the severity of ceramic fractures. Clin Oral Investig. 2015; 19:2295–2307.
Article10. Rinke S, Kramer K, Bürgers R, Roediger M. A practice-based clinical evaluation of the survival and success of metal-ceramic and zirconia molar crowns: 5-year results. J Oral Rehabil. 2016; 43:136–144. PMID: 26393865.
Article11. Ortorp A, Kihl ML, Carlsson GE. A 5-year retrospective study of survival of zirconia single crowns fitted in a private clinical setting. J Dent. 2012; 40:527–530. PMID: 22387979.12. Ryge G, Snyder M. Evaluating the clinical quality of restorations. J Am Dent Assoc. 1973; 87:369–377. PMID: 4515696.
Article13. Eisenburger M, Tschernitschek H. Clinical and technical comparison of the long term success of clasp retained dentures and of telescopic crown retained dentures. Dtsch Zahnärzl Z. 1998; 53:257–259.14. Beuer F, Sachs C, Groesser J, Gueth JF, Stimmelmayr M. Tooth-implant-supported posterior fixed dental prostheses with zirconia frameworks: 3-year clinical result. Clin Oral Investig. 2016; 20:1079–1086.
Article15. Raigrodski AJ, Hillstead MB, Meng GK, Chung KH. Survival and complications of zirconia-based fixed dental prostheses: a systematic review. J Prosthet Dent. 2012; 107:170–177. PMID: 22385693.
Article16. Raigrodski AJ, Yu A, Chiche GJ, Hochstedler JL, Mancl LA, Mohamed SE. Clinical efficacy of veneered zirconium dioxide-based posterior partial fixed dental prostheses: five-year results. J Prosthet Dent. 2012; 108:214–222. PMID: 23031727.
Article17. Hey J, Beuer F, Bensel T, Boeckler AF. Single crowns with CAD/CAM-fabricated copings from titanium: 6-year clinical results. J Prosthet Dent. 2014; 112:150–154. PMID: 24529840.
Article18. Prabhu R, Prabhu G, Baskaran E, Arumugam EM. Clinical acceptability of metal-ceramic fixed partial dental prosthesis fabricated with direct metal laser sintering technique-5 year follow-up. J Indian Prosthodont Soc. 2016; 16:193–197. PMID: 27141171.
Article19. Sailer I, Makarov NA, Thoma DS, Zwahlen M, Pjetursson BE. All-ceramic or metal-ceramic tooth-supported fixed dental prostheses (FDPs)? A systematic review of the survival and complication rates. Part I: Single crowns (SCs). Dent Mater. 2015; 31:603–623. PMID: 25842099.
Article20. Pjetursson BE, Brägger U, Lang NP, Zwahlen M. Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin Oral Implants Res. 2007; 18:97–113. PMID: 17594374.
Article21. Sax C, Hämmerle CH, Sailer I. 10-year clinical outcomes of fixed dental prostheses with zirconia frameworks. Int J Comput Dent. 2011; 14:183–202. PMID: 22141229.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A study on the fracture strength of collarless metal-ceramic fixed partial dentures
- Marginal fit of anterior 3-unit fixed partial zirconia restorations using different CAD/CAM systems
- A study on the marginal fit of collarless metal ceramic fixed partial dentures
- Clinical performance and failures of zirconia-based fixed partial dentures: a review literature
- Real-World Impact of Modern Reperfusion Therapy for Acute Ischemic Stroke : A Nationwide Population-Based Data Study in Korea