Cancer Res Treat.
2015 Oct;47(4):931-936. 10.4143/crt.2014.049.
Conventional Cisplatin-Based Combination Chemotherapy Is Effective in the Treatment of Metastatic Spermatocytic Seminoma with Extensive Rhabdomyosarcomatous Transformation
- Affiliations
-
- 1Department of Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. jaelyun@amc.seoul.kr
- 2Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 3Department of Urology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 4Department of Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2403414
- DOI: http://doi.org/10.4143/crt.2014.049
Abstract
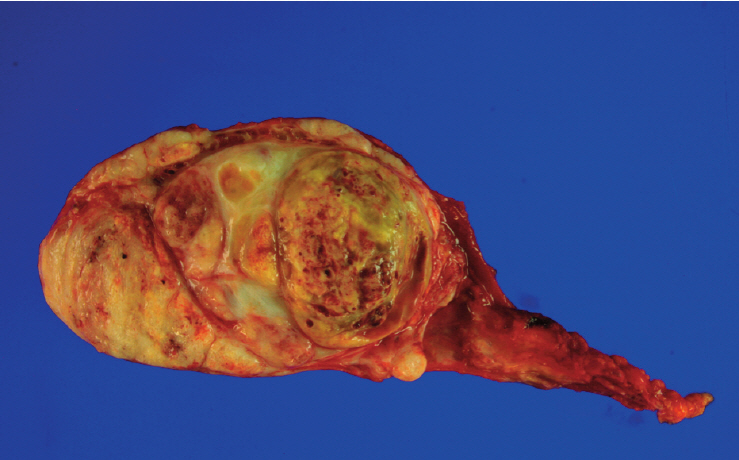
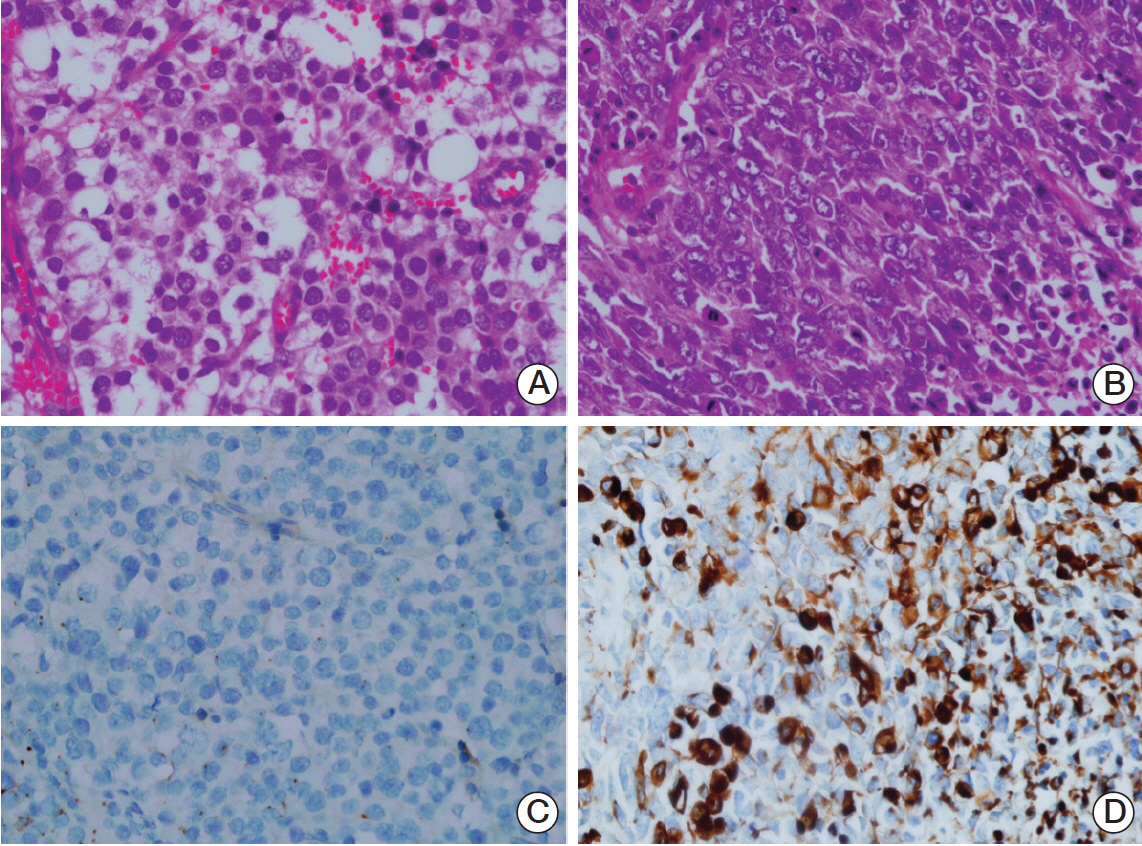
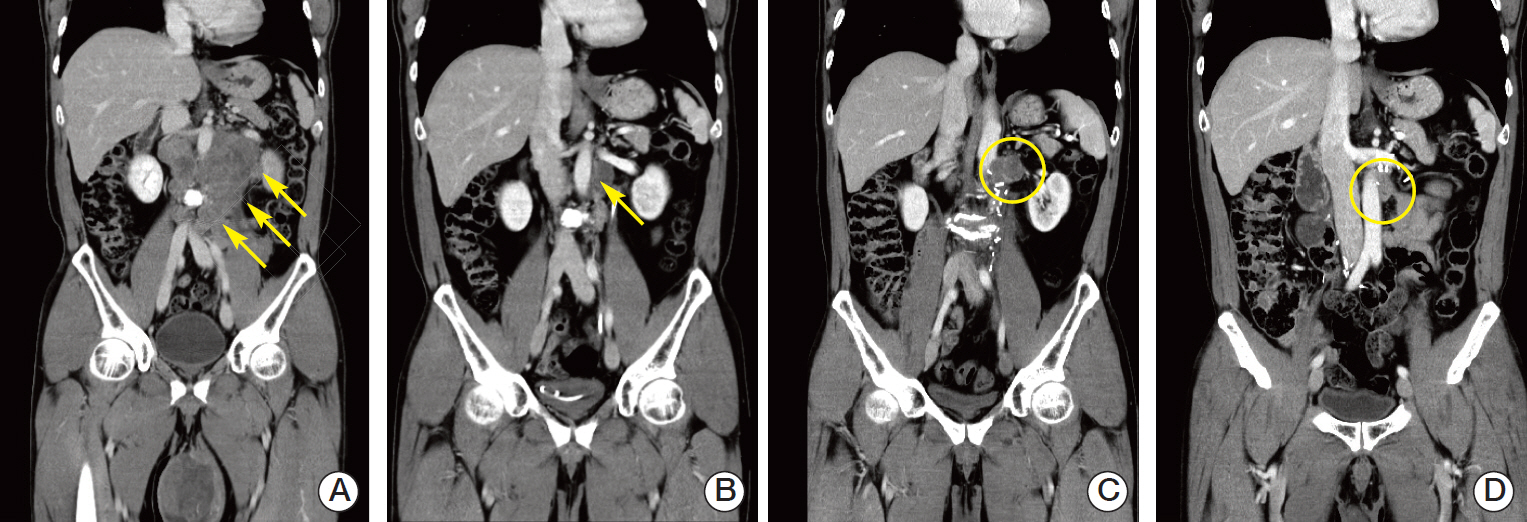
- A 52-year-old man was presented with a huge left testicular mass and palpable cervical lymphadenopathy with retroperitoneal lymph node enlargement on an abdominal computed tomography. A left radical orchiectomy and an ultrasound-guided neck node biopsy were performed. A pathological examination revealed spermatocytic seminoma with extensive rhabdomyosarcomatous transformation, a condition known to be highly resistant to platinum-based chemotherapy. The patient received four cycles of etoposide, ifosfamide and cisplatin (VIP) chemotherapy. A repeat computed tomography revealed a substantial regression consistent with a partial response. Retroperitoneal lymph node dissection was attempted, which revealed rhabdomyosarcoma; however, complete microscopic resection was not achieved. After surgery, the residual abdominal lymph node progressed and salvage paclitaxel, ifosfamide and cisplatin (TIP) chemotherapy was employed, which again achieved a partial response. Here, we present a first case report of a spermatocytic seminoma with extensive rhabdomyosarcomatous transformation and multiple metastatic lymphadenopathies that showed a favorable response to platinum-based systemic chemotherapy.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Talerman A. Spermatocytic seminoma: clinicopathological study of 22 cases. Cancer. 1980; 45:2169–76.
Article2. Chelly I, Mekni A, Gargouri MM, Bellil K, Zitouna M, Horchani A, et al. Spermatocytic seminoma with rhadomyosarcomatous contingent. Prog Urol. 2006; 16:218–20.3. Matoska J, Talerman A. Spermatocytic seminoma associated with rhabdomyosarcoma. Am J Clin Pathol. 1990; 94:89–95.
Article4. Malagon HD, Valdez AM, Moran CA, Suster S. Germ cell tumors with sarcomatous components: a clinicopathologic and immunohistochemical study of 46 cases. Am J Surg Pathol. 2007; 31:1356–62.5. Wetherell D, Lawrentschuk N, Gyomber D. Spermatocytic seminoma with sarcoma: an indication for adjuvant chemotherapy in localized disease. Korean J Urol. 2013; 54:884–7.
Article6. Masson P. A study of seminomas. Rev Can Biol. 1946; 5:361–87.7. Chung PW, Bayley AJ, Sweet J, Jewett MA, Tew-George B, Gospodarowicz MK, et al. Spermatocytic seminoma: a review. Eur Urol. 2004; 45:495–8.
Article8. True LD, Otis CN, Rosai J, Scully RE, Delprado W. Spermatocytic seminoma of testis with sarcomatous transformation. Am J Surg Pathol. 1988; 12:806.
Article9. Trivedi P, Pasricha S, Gupta A. Spermatocytic seminoma associated with undifferentiated sarcoma: a rare case report. Indian J Pathol Microbiol. 2011; 54:138–40.
Article10. Robinson A, Bainbridge T, Kollmannsberger C. A spermatocytic seminoma with rhabdomyosarcoma transformation and extensive metastases. Am J Clin Oncol. 2007; 30:440–1.
Article11. Floyd C, Ayala AG, Logothetis CJ, Silva EG. Spermatocytic seminoma with associated sarcoma of the testis. Cancer. 1988; 61:409–14.
Article12. Duchesne GM, Stenning SP, Aass N, Mead GM, Fossa SD, Oliver RT, et al. Radiotherapy after chemotherapy for metastatic seminoma: a diminishing role. MRC Testicular Tumour Working Party. Eur J Cancer. 1997; 33:829–35.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spermatocytic Seminoma With Sarcoma: An Indication for Adjuvant Chemotherapy in Localized Disease
- Etoposide and cisplatin combination chemotherapy in extensive stage small cell lung cancer
- A Comparative study of Cyclophophamide and Cisplatin with or without Doxorubicin in Ovarian Carcinoma
- A Case of Systemic Chemetherapy in Advanced Seminoma
- Adjuvant Chemotherapy in Gastric Cancer