Ann Lab Med.
2018 Mar;38(2):102-109. 10.3343/alm.2018.38.2.102.
Increasing Incidence of Listeriosis and Infection-associated Clinical Outcomes
- Affiliations
-
- 1Department of Laboratory Medicine and Research Institute of Bacterial Resistance, Yonsei University College of Medicine, Seoul, Korea. leekcp@yuhs.ac
- 2Department of Laboratory Medicine, National Health Insurance Service Ilsan Hospital, Goyang, Korea.
- 3Department of Internal Medicine and AIDS Research Institute, Yonsei University College of Medicine, Seoul, Korea. seran@yuhs.ac
- KMID: 2403354
- DOI: http://doi.org/10.3343/alm.2018.38.2.102
Abstract
- BACKGROUND
Listeriosis caused by Listeria monocytogenes has a high case-fatality rate (CFR) of approximately 20% to 30%. An increasing incidence of listeriosis has been reported in many countries recently. We investigated the annual incidence, clinical characteristics, and outcomes of listeriosis at three different hospitals in Korea and evaluated the effects of appropriate empiric antimicrobial treatments on patient outcomes.
METHODS
We retrospectively collected the data of all culture-positive cases of human listeriosis from three hospitals of different sizes in Korea during 2006-2016 and calculated the annual number of cases and incidence per 100,000 admissions.
RESULTS
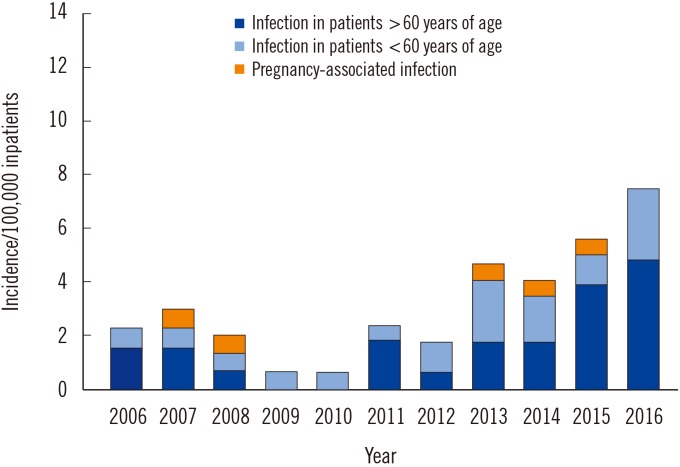
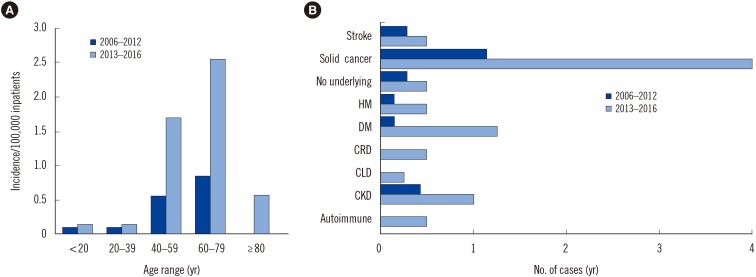
A total of 58 patients with L. monocytogenes were included in this study. The incidence of listeriosis was significantly higher in 2013-2016 than in 2006-2012 (RR 3.1; 95% CI 1.79-5.36; P < 0.001), mainly because of an increase in patients over 60 years of age (RR 3.69; 95% CI 1.70-8.02; P < 0.001). Multivariate analysis showed that healthcare-associated infection (adjusted OR, 12.15; 95% CI, 2.56-86.01; P=0.004) and empirical treatment with first-line antimicrobial agents (adjusted OR, 0.08; 95% CI, 0.00-0.63; P=0.044) were associated with CFR.
CONCLUSIONS
Healthcare-associated infections caused by L. monocytogenes are associated with high CFR. Adequate initial empirical treatments could reduce CFR, suggesting that careful consideration of an empirical antimicrobial regimen is warranted for elderly or immunocompromised patients admitted to the hospital.
MeSH Terms
Figure
Cited by 1 articles
-
Listeriosis in a Pregnant Woman and a Neonate
Ha Young Yun, Juhui Kim, Su Jin Cho, Eun Ae Park, Young Ju Kim, Sunwha Park
Ewha Med J. 2020;43(4):60-64. doi: 10.12771/emj.2020.43.4.60.
Reference
-
1. Jensen AK, Bjorkman JT, Ethelberg S, Kiil K, Kemp M, Nielsen EM. Molecular typing and epidemiology of human listeriosis cases, Denmark, 2002-2012. Emerg Infect Dis. 2016; 22:625–633. PMID: 26982714.2. Carpentier B, Cerf O. Review--Persistence of Listeria monocytogenes in food industry equipment and premises. Int J Food Microbiol. 2011; 145:1–8. PMID: 21276634.3. Barton Behravesh C, Jones TF, Vugia DJ, Long C, Marcus R, Smith K, et al. Deaths associated with bacterial pathogens transmitted commonly through food: foodborne diseases active surveillance network (FoodNet), 1996-2005. J Infect Dis. 2011; 204:263–267. PMID: 21673037.4. Koopmans MM, Brouwer MC, Bijlsma MW, Bovenkerk S, Keijzers W, van der Ende A, et al. Listeria monocytogenes sequence type 6 and increased rate of unfavorable outcome in meningitis: epidemiologic cohort study. Clin Infect Dis. 2013; 57:247–253. PMID: 23592828.5. Kerouanton A, Roche SM, Marault M, Velge P, Pourcher AM, Brisabois A, et al. Characterization of isolates of Listeria monocytogenes from sludge using pulsed-field gel electrophoresis and virulence assays. J Appl Microbiol. 2010; 108:1380–1388. PMID: 19796096.6. Ragon M, Wirth T, Hollandt F, Lavenir R, Lecuit M, Le Monnier A, et al. A new perspective on Listeria monocytogenes evolution. PLoS Pathog. 2008; 4:e1000146. PMID: 18773117.7. Miya S, Takahashi H, Nakagawa M, Kuda T, Igimi S, Kimura B. Genetic characteristics of Japanese clinical Listeria monocytogenes isolates. PLoS One. 2015; 10:e0122902. PMID: 25826318.8. Park S, Jung J, Choi S, Oh Y, Lee J, Chae H, et al. Molecular characterization of Listeria monocytogenes based on the PFGE and RAPD in Korea. Adv Microbiol. 2012; 02:605–616.9. Zunabovic M, Domig KJ, Kneifel W. Practical relevance of methodologies for detecting and tracing of Listeria monocytogenes in ready-to-eat foods and manufacture environments – A review. LWT–Food Sci Technol. 2011; 44:351–362.10. Allerberger F, Wagner M. Listeriosis: a resurgent foodborne infection. Clin Microbiol Infect. 2010; 16:16–23. PMID: 20002687.11. Lee CY, Tsai HC, Kunin CM, Lee SS, Wu KS, Chen YS. Emergence of sporadic non-clustered cases of hospital-associated listeriosis among immunocompromised adults in southern Taiwan from 1992 to 2013: effect of precipitating immunosuppressive agents. BMC Infect Dis. 2014; 14:145. PMID: 24641498.12. Hedberg C. Listeria in Europe: the need for a European surveillance network is growing. Euro Surveill. 2006; 11:75–76. PMID: 16801698.13. Cartwright EJ, Jackson KA, Johnson SD, Graves LM, Silk BJ, Mahon BE. Listeriosis outbreaks and associated food vehicles, United States, 1998-2008. Emerg Infect Dis. 2013; 19:1–9. quiz 184. PMID: 23260661.14. Jadhav S, Bhave M, Palombo EA. Methods used for the detection and subtyping of Listeria monocytogenes. J Microbiol Methods. 2012; 88:327–341. PMID: 22261140.15. Bertrand S, Ceyssens PJ, Yde M, Dierick K, Boyen F, Vanderpas J, et al. Diversity of Listeria monocytogenes strains of clinical and food chain origins in Belgium between 1985 and 2014. PLoS One. 2016; 11:e0164283. PMID: 27723768.16. Wang Y, Zhao A, Zhu R, Lan R, Jin D, Cui Z, et al. Genetic diversity and molecular typing of Listeria monocytogenes in China. BMC Microbiol. 2012; 12:119. PMID: 22727037.17. Wang HL, Ghanem KG, Wang P, Yang S, Li TS. Listeriosis at a tertiary care hospital in Beijing, China: high prevalence of nonclustered healthcare-associated cases among adult patients. Clin Infect Dis. 2013; 56:666–676. PMID: 23175565.18. Silk BJ, McCoy MH, Iwamoto M, Griffin PM. Foodborne listeriosis acquired in hospitals. Clin Infect Dis. 2014; 59:532–540. PMID: 24846635.19. Mylonakis E, Hohmann EL, Calderwood SB. Central nervous system infection with Listeria monocytogenes. 33 years’ experience at a general hospital and review of 776 episodes from the literature. Medicine (Baltimore). 1998; 77:313–336. PMID: 9772921.20. Blanot S, Boumaila C, Berche P. Intracerebral activity of antibiotics against Listeria monocytogenes during experimental rhombencephalitis. J Antimicrob Chemother. 1999; 44:565–568. PMID: 10588323.21. Goulet V, Hedberg C, Le Monnier A, de Valk H. Increasing incidence of listeriosis in France and other European countries. Emerg Infect Dis. 2008; 14:734–740. PMID: 18439354.22. Stahlmann R, Lode HM. Risks associated with the therapeutic use of fluoroquinolones. Expert Opin Drug Saf. 2013; 12:497–505. PMID: 23651367.23. Leazer R, Perkins AM, Shomaker K, Fine B. A meta-analysis of the rates of Listeria monocytogenes and enterococcus in febrile infants. Hosp Pediatr. 2016; 6:187–195. PMID: 26980752.24. Girard D, Leclercq A, Laurent E, Lecuit M, de Valk H, Goulet V. Pregnancy-related listeriosis in France, 1984 to 2011, with a focus on 606 cases from 1999 to 2011. Euro Surveill. 2014; 19.25. Tappero JW, Schuchat A, Deaver KA, Mascola L, Wenger JD. Reduction in the incidence of human listeriosis in the United States. Effectiveness of prevention efforts? The Listeriosis Study Group. JAMA. 1995; 273:1118–1122. PMID: 7707600.26. Awofisayo A, Amar C, Ruggles R, Elson R, Adak GK, Mook P, et al. Pregnancy-associated listeriosis in England and Wales. Epidemiol Infect. 2015; 143:249–256. PMID: 24650375.27. Pouillot R, Hoelzer K, Jackson KA, Henao OL, Silk BJ. Relative risk of listeriosis in Foodborne Diseases Active Surveillance Network (FoodNet) sites according to age, pregnancy, and ethnicity. Clin Infect Dis. 2012; 54(Suppl 5):S405–S410. PMID: 22572661.28. Cantinelli T, Chenal-Francisque V, Diancourt L, Frezal L, Leclercq A, Wirth T, et al. “Epidemic clones” of Listeria monocytogenes are widespread and ancient clonal groups. J Clin Microbiol. 2013; 51:3770–3779. PMID: 24006010.29. Haase JK, Didelot X, Lecuit M, Korkeala H, Achtman M. The ubiquitous nature of Listeria monocytogenes clones: a large-scale Multilocus Sequence Typing study. Environ Microbiol. 2014; 16:405–416. PMID: 24274459.30. Verghese B, Lok M, Wen J, Alessandria V, Chen Y, Kathariou S, et al. comK prophage junction fragments as markers for Listeria monocytogenes genotypes unique to individual meat and poultry processing plants and a model for rapid niche-specific adaptation, biofilm formation, and persistence. Appl Environ Microbiol. 2011; 77:3279–3292. PMID: 21441318.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Increasing Incidence of Listeriosis and Infection associated Clinical Outcomes
- Neonatal Listeriosis with Granulomatosis Infantiseptica: A Case Report
- Listeriosis in baby and mother confirmed with blood and amniotic fluid cultures
- Food borne illness-Salmonellosis, Virbriosis, Listeriosis
- Challenging management of chorioamnionitis with placental listeriosis: lessons from 2 cases