Healthc Inform Res.
2018 Jan;24(1):29-37. 10.4258/hir.2018.24.1.29.
Comparison of Models for the Prediction of Medical Costs of Spinal Fusion in Taiwan Diagnosis-Related Groups by Machine Learning Algorithms
- Affiliations
-
- 1Institute of Information Management, Yuan-Ze University, Taoyuan, Taiwan. clchan@saturn.yzu.edu.tw
- 2Department of Medical Administration, Taoyuan General Hospital, Ministry of Health and Welfare, Taoyuan, Taiwan.
- 3Department of Orthopedics, Taoyuan General Hospital, Ministry of Health and Welfare, Taoyuan, Taiwan.
- 4Innovation Center for Big Data and Digital Convergence, Yuan-Ze University, Taoyuan, Taiwan.
- KMID: 2403293
- DOI: http://doi.org/10.4258/hir.2018.24.1.29
Abstract
OBJECTIVES
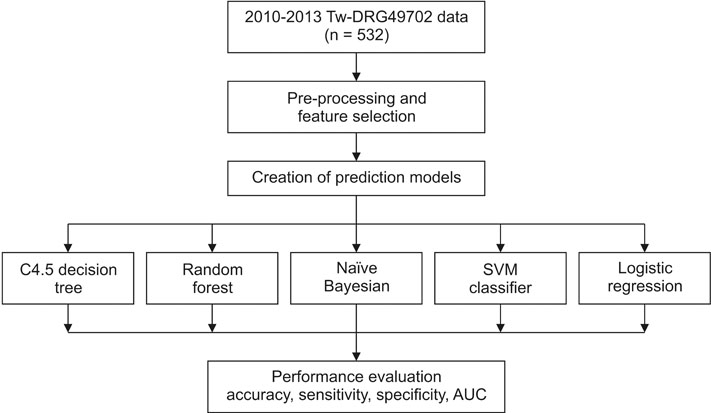
The aims of this study were to compare the performance of machine learning methods for the prediction of the medical costs associated with spinal fusion in terms of profit or loss in Taiwan Diagnosis-Related Groups (Tw-DRGs) and to apply these methods to explore the important factors associated with the medical costs of spinal fusion.
METHODS
A data set was obtained from a regional hospital in Taoyuan city in Taiwan, which contained data from 2010 to 2013 on patients of Tw-DRG49702 (posterior and other spinal fusion without complications or comorbidities). Naïve-Bayesian, support vector machines, logistic regression, C4.5 decision tree, and random forest methods were employed for prediction using WEKA 3.8.1.
RESULTS
Five hundred thirty-two cases were categorized as belonging to the Tw-DRG49702 group. The mean medical cost was US $4,549.7, and the mean age of the patients was 62.4 years. The mean length of stay was 9.3 days. The length of stay was an important variable in terms of determining medical costs for patients undergoing spinal fusion. The random forest method had the best predictive performance in comparison to the other methods, achieving an accuracy of 84.30%, a sensitivity of 71.4%, a specificity of 92.2%, and an AUC of 0.904.
CONCLUSIONS
Our study demonstrated that the random forest model can be employed to predict the medical costs of Tw-DRG49702, and could inform hospital strategy in terms of increasing the financial management efficiency of this operation.
MeSH Terms
Figure
Cited by 2 articles
-
Using Statistical and Machine Learning Methods to Evaluate the Prognostic Accuracy of SIRS and qSOFA
Akash Gupta, Tieming Liu, Scott Shepherd, William Paiva
Healthc Inform Res. 2018;24(2):139-147. doi: 10.4258/hir.2018.24.2.139.Fast Convolutional Method for Automatic Sleep Stage Classification
Intan Nurma Yulita, Mohamad Ivan Fanany, Aniati Murni Arymurthy
Healthc Inform Res. 2018;24(3):170-178. doi: 10.4258/hir.2018.24.3.170.
Reference
-
1. Rajaee SS, Bae HW, Kanim LE, Delamarter RB. Spinal fusion in the United States: analysis of trends from 1998 to 2008. Spine (Phila Pa 1976). 2012; 37(1):67–76.2. Jancuska JM, Hutzler L, Protopsaltis TS, Bendo JA, Bosco J. Utilization of lumbar spinal fusion in New York State: trends and disparities. Spine (Phila Pa 1976). 2016; 41(19):1508–1514.3. Rimler SB, Gale BD, Reede DL. Diagnosis-related groups and hospital inpatient federal reimbursement. Radiographics. 2015; 35(6):1825–1834.
Article4. Hsiao WC, Sapolsky HM, Dunn DL, Weiner SL. Lessons of the New Jersey DRG payment system. Health Aff (Millwood). 1986; 5(2):32–45.
Article5. Ugiliweneza B, Kong M, Nosova K, Huang KT, Babu R, Lad SP, et al. Spinal surgery: variations in health care costs and implications for episode-based bundled payments. Spine (Phila Pa 1976). 2014; 39(15):1235–1242.6. Wright DJ, Mukamel DB, Greenfield S, Bederman SS. Cost variation within spinal fusion payment groups. Spine (Phila Pa 1976). 2016; 41(22):1747–1753.
Article7. National Health Research Institutes. Background of National Health Insurance Research Database in Taiwan [Internet]. Miaoli County, Taiwan: National Health Research Institutes;c2016. cited at 2018 Jan 10. Available from: http://nhird.nhri.org.tw/en/index.html.8. Taiwan National Health Insurance Administration. DRG payment system 2017 [Internet]. Taipei, Taiwan: National Health Insurance Administration;c2017. cited at 2018 Jan 10. Available from: https://www.nhi.gov.tw/Content_List.aspx?n=9261941716EB8070&topn=CA428784F9ED78C9.9. Tomar D, Agarwal S. A survey on data mining approaches for healthcare. Int J Biosci Biotechnol. 2013; 5(5):241–266.
Article10. Moon M, Lee SK. Applying of decision tree analysis to risk factors associated with pressure ulcers in long-term care facilities. Healthc Inform Res. 2017; 23(1):43–52.
Article11. Yahya N, Ebert MA, Bulsara M, House MJ, Kennedy A, Joseph DJ, et al. Statistical-learning strategies generate only modestly performing predictive models for urinary symptoms following external beam radiotherapy of the prostate: a comparison of conventional and machine-learning methods. Med Phys. 2016; 43(5):2040–2052.
Article12. Walid MS, Robinson JS Jr. Economic impact of comorbidities in spine surgery. J Neurosurg Spine. 2011; 14(3):318–321.
Article13. Chawla NV, Bowyer KW, Hall LO, Kegelmeyer WP. SMOTE: synthetic minority over-sampling technique. J Artif Intell Res. 2002; 16:321–357.
Article14. Han J, Kamber M, Pei J. Data mining: concepts and techniques. 3rd ed. Amsterdam: Elsevier;2011.15. Miranda E, Irwansyah E, Amelga AY, Maribondang MM, Salim M. Detection of cardiovascular disease risk's level for adults using naive Bayes classifier. Healthc Inform Res. 2016; 22(3):196–205.
Article16. à Cortes C, Vapnik V. Support-vector networks. Machine Learning. 1995; 20(3):273–297.
Article17. Kuo PJ, Wu SC, Chien PC, Rau CS, Chen YC, Hsieh HY, et al. Derivation and validation of different machine-learning models in mortality prediction of trauma in motorcycle riders: a cross-sectional retrospective study in southern Taiwan. BMJ Open. 2018; 8(1):e018252.
Article18. Quinlan JR. Induction of decision trees. Mach Learn. 1986; 1(1):81–106.
Article19. Archana S, Elangovan K. Survey of classification techniques in data mining. Int J Comput Sci Mob Appl. 2014; 2(2):65–71.20. Sanz J, Paternain D, Galar M, Fernandez J, Reyero D, Belzunegui T. A new survival status prediction system for severe trauma patients based on a multiple classifier system. Comput Methods Programs Biomed. 2017; 142:1–8.
Article21. Habibi S, Ahmadi M, Alizadeh S. Type 2 diabetes mellitus screening and risk factors using decision tree: results of data mining. Glob J Health Sci. 2015; 7(5):304–310.
Article22. Breiman L. Random forests. Mach Learn. 2001; 45(1):5–32.23. Raju D, Su X, Patrician PA, Loan LA, McCarthy MS. Exploring factors associated with pressure ulcers: a data mining approach. Int J Nurs Stud. 2015; 52(1):102–111.
Article24. Bellazzi R, Zupan B. Predictive data mining in clinical medicine: current issues and guidelines. Int J Med Inform. 2008; 77(2):81–97.
Article25. Bradywood A, Farrokhi F, Williams B, Kowalczyk M, Blackmore CC. Reduction of inpatient hospital length of stay in lumbar fusion patients with implementation of an evidence-based clinical care pathway. Spine (Phila Pa 1976). 2017; 42(3):169–176.
Article26. Kulkarni VY, Sinha PK. Random forest classifiers: a survey and future research directions. Int J Adv Comput. 2013; 36(1):1144–1153.27. Hu H, Li J, Plank A, Wang H, Daggard G. A comparative study of classification methods for microarray data analysis. In : Proceedings of the 5th Australasian Conference on Data Mining and Analystics; 2006 Nov 29; Sydney, Australia. p. 33–37.28. Masetic Z, Subasi A. Congestive heart failure detection using random forest classifier. Comput Methods Programs Biomed. 2016; 130:54–64.
Article29. Allyn J, Allou N, Augustin P, Philip I, Martinet O, Belghiti M, et al. A comparison of a machine learning model with EuroSCORE II in predicting mortality after elective cardiac surgery: a decision curve analysis. PLoS One. 2017; 12(1):e0169772.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Predictive Modeling of Outcomes After Traumatic and Nontraumatic Spinal Cord Injury Using Machine Learning: Review of Current Progress and Future Directions
- Prediction of dental caries in 12-year-old children using machine-learning algorithms
- Machine Learning vs. Statistical Model for Prediction Modelling: Application in Medical Imaging Research
- Machine Learning and Deep Learning for the Pharmacogenomics of Antidepressant Treatments
- A Hybrid Machine Learning Approach To the Promoter Prediction Problem