Allergy Asthma Respir Dis.
2018 Jan;6(1):72-76. 10.4168/aard.2018.6.1.72.
Eosinophilic granulomatosis with polyangiitis presenting with acutepolyneuropathy mimicking Guillain-Barré syndrome: A case report
- Affiliations
-
- 1Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea. jhj0619061@yu.ac.kr
- KMID: 2403189
- DOI: http://doi.org/10.4168/aard.2018.6.1.72
Abstract
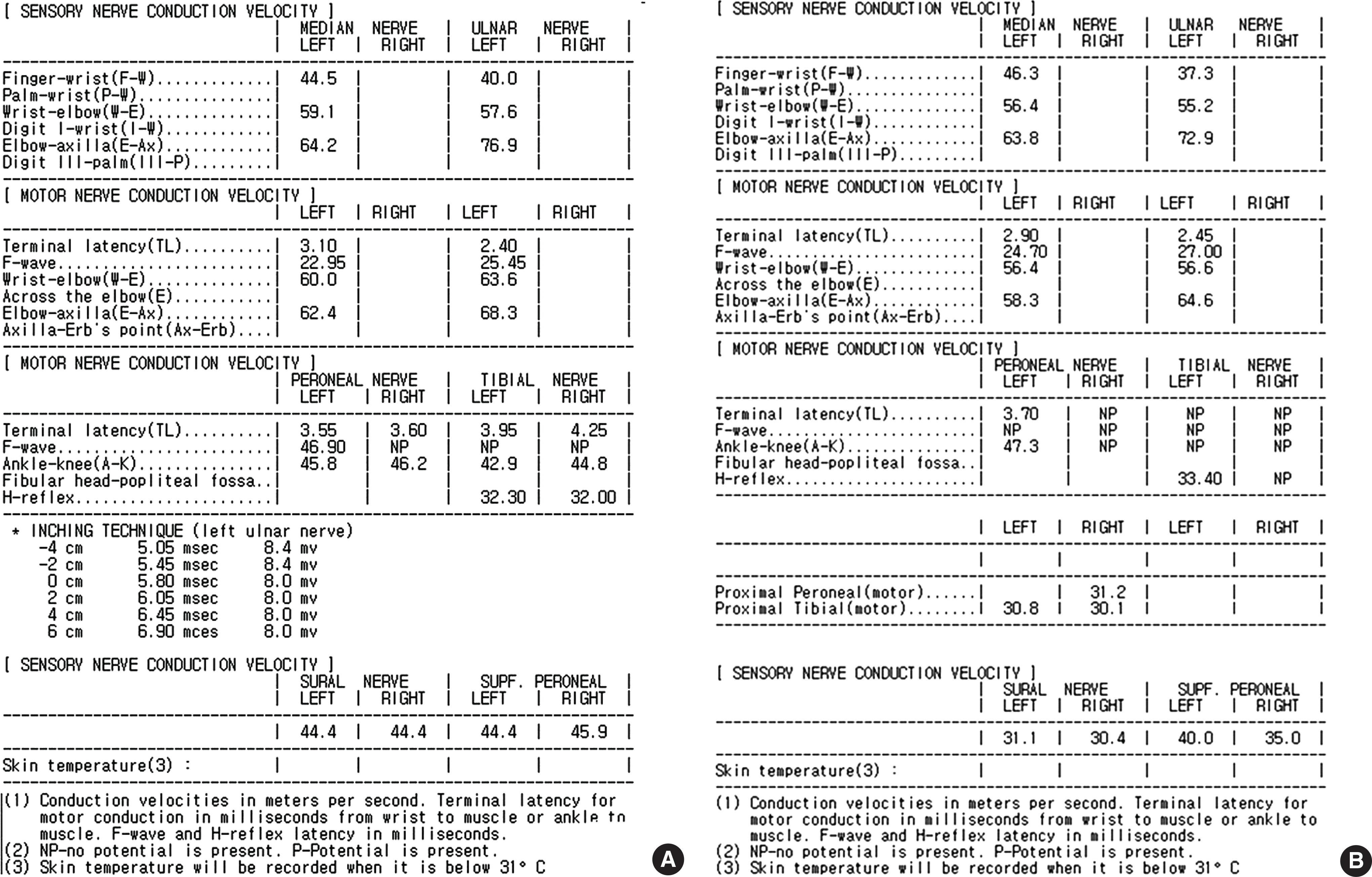
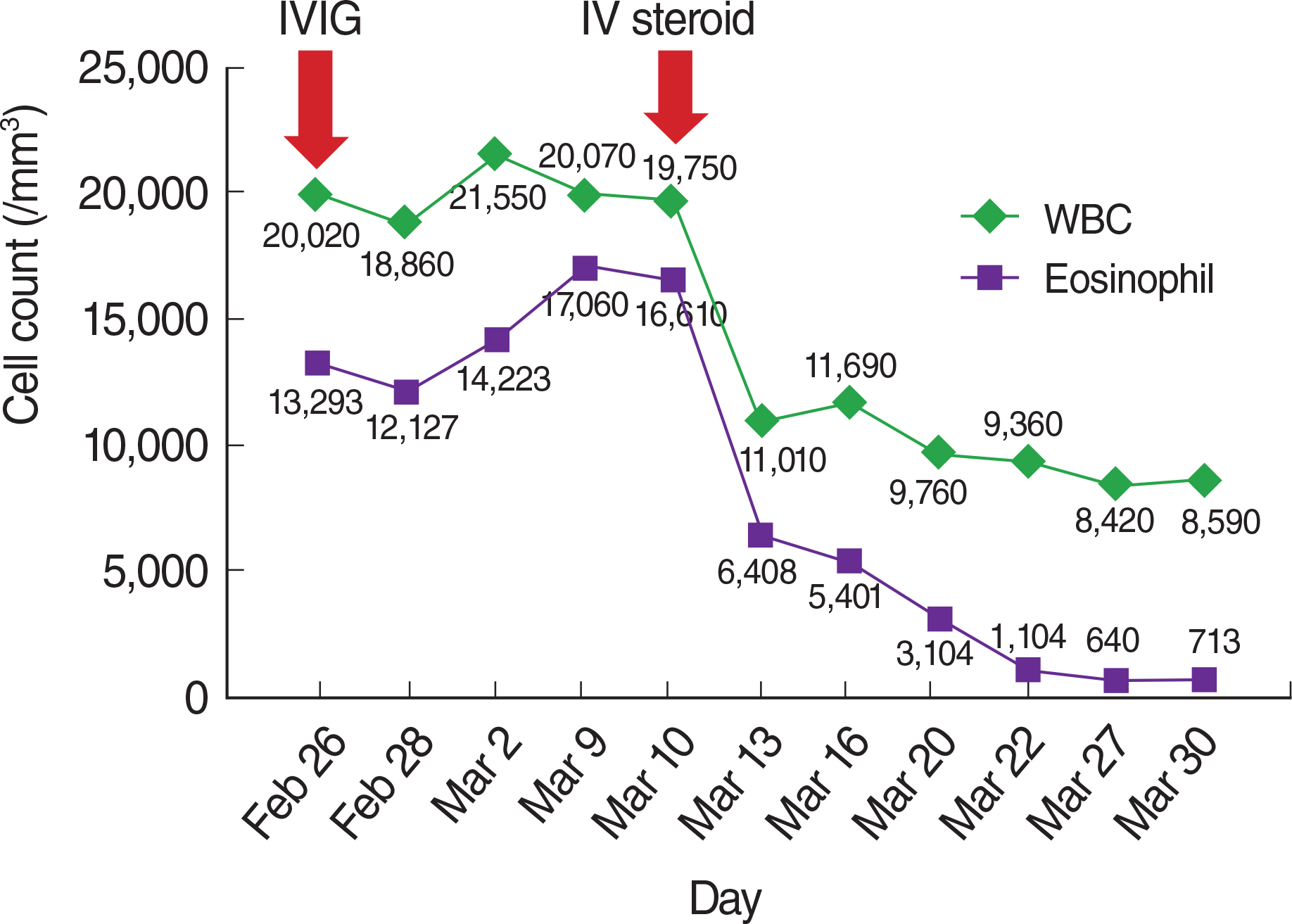
- Eosinophilic granulomatosis with polyangiitis (EGPA) is a rare systemic vasculitis that commonly affects the peripheral nervous system. EGPA rarely presents with acute polyneuropathy resembling Guillain-Barré syndrome (GBS). A 51-year-old female patient with a history of asthma suddenly developed bilateral lower extremityparesthesia that progressed to asymmetric ascending paralysis within 10 days of onset. Nerve conduction study results were compatible with acute motor sensory axonal neuropathy, consistent with a GBS subtype. A clinical and neurophysiological diagnosis of GBS was made, and high-dose intravenous immunoglobulins were administered. However, the patient's painful motor weakness persisted. Furthermore, she had newly developed skin lesions on her back, face, and arms. Her blood test revealed marked eosinophilia (>60%). In addition, antineutrophil cytoplasmic antibodies were reported positive. A Water's view radiographic image showed bilateral maxillary sinusitis. Considering the history of asthma, we suspected EGPA-associated polyneuropathy and started steroid treatment. The patient's strength and eosinophilia improved rapidly and dramatically. EGPA can mimic GBS and should be differentiated because of different treatment strategies. Early diagnosis and prompt treatment help achieve a good outcome.
MeSH Terms
-
Antibodies, Antineutrophil Cytoplasmic
Arm
Asthma
Axons
Diagnosis
Early Diagnosis
Eosinophilia
Eosinophils*
Female
Granulomatosis with Polyangiitis*
Guillain-Barre Syndrome*
Hematologic Tests
Humans
Immunoglobulins, Intravenous
Maxillary Sinus
Maxillary Sinusitis
Middle Aged
Neural Conduction
Paralysis
Peripheral Nervous System
Polyneuropathies
Skin
Systemic Vasculitis
Antibodies, Antineutrophil Cytoplasmic
Immunoglobulins, Intravenous
Figure
Reference
-
1. Churg J, Strauss L. Allergic granulomatosis, allergic angiitis, and periar-teritis nodosa. Am J Pathol. 1951; 27:277–301.2. Noth O, Strek ME, Leff AR. Churg-Strauss syndrome. Lancet. 2003; 361:587–94.
Article3. Kang DW, Jeong IK, Kim HJ, Lee KW. Neurologic manifestations of Churg-Strauss syndrome. J Korean Neurol Assoc. 1999; 17:836–40.4. Yi JS, Jung HY, Choi SW. A case of acute fulminant neuropathy in patient with allergic granulomatosis and angiitis. J Korean Rheum Assoc. 1998; 5:298–302.5. Oh MJ, Lee JY, Kwon NH, Choi DC. Churg-Strauss syndrome: the clinical features and long-term follow-up of 17 patients. J Korean Med Sci. 2006; 21:265–71.
Article6. Camara-Lemarroy CR, Infante-Valenzuela A, Villareal-Montemayor HJ, Soto-Rincon CA, Davila-Olalde JA, Villareal-Velazquez HJ. Eosinophilic granulomatosis with polyangiitis presenting as acute polyneuropathy mimicking Guillain-Barre syndrome. Case Rep Neurol Med. 2015; 2015:981439.
Article7. Cho HJ, Yune S, Seok JM, Cho EB, Min JH, Seo YL, et al. Clinical characteristics and treatment response of peripheral neuropathy in the presence of eosinophilic granulomatosis with polyangiitis (Churg-Strauss Syndrome): experience at a single tertiary center. J Clin Neurol. 2017; 13:77–83.
Article8. Santos-Pinheiro F, Li Y. Eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome) presenting with polyneuropathy: a case series. J Clin Neuromuscul Dis. 2015; 16:125–30.9. Seok JI, Bae JS, Joo EY, Min TH, Choi DC, Kim BJ. Clinical and electro-physiologic features of peripheral neuropathy in Churg-Strauss syndrome. J Korean Neurol Assoc. 2004; 22:127–33.10. Jamieson PW, Giuliani MJ, Martinez AJ. Necrotizing angiopathy presenting with multifocal conduction blocks. Neurology. 1991; 41:442–4.
Article11. Winer JB. An update in guillain-barré syndrome. Autoimmune Dis. 2014; 2014:793024.
Article13. Masi AT, Hunder GG, Lie JT, Michel BA, Bloch DA, Arend WP, et al. The American College of Rheumatology 1990 criteria for the classification of Churg-Strauss syndrome (allergic granulomatosis and angiitis). Arthritis Rheum. 1990; 33:1094–100.
Article14. Giusti Del Giardino L, Cavallaro T, Anzola GP, Lombardi C, Ferrari S. Neuropathy in eosinophilic granulomatosis with polyangiitis: a comparison study of 24 cases with or without prior leukotriene antagonist exposure. Eur Ann Allergy Clin Immunol. 2014; 46:201–9.15. Ribi C, Cohen P, Pagnoux C, Mahr A, Arène JP, Lauque D, et al. Treatment of Churg-Strauss syndrome without poor-prognosis factors: a multicenter, prospective, randomized, open-label study of seventy-two patients. Arthritis Rheum. 2008; 58:586–94.
Article16. Guillevin L, Lhote F, Gayraud M, Cohen P, Jarrousse B, Lortholary O, et al. Prognostic factors in polyarteritis nodosa and Churg-Strauss syndrome. A prospective study in 342 patients. Medicine (Baltimore). 1996; 75:17–28.
Article17. Koike H, Akiyama K, Saito T, Sobue G. Research Group for IVIg for EGPA/CSS in Japan. Intravenous immunoglobulin for chronic residual peripheral neuropathy in eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome): a multicenter, double-blind trial. J Neurol. 2015; 262:752–9.
Article18. Hattori N, Ichimura M, Nagamatsu M, Li M, Yamamoto K, Kumazawa K, et al. Clinicopathological features of Churg-Strauss syndrome-associated neuropathy. Brain. 1999; 122(Pt 3):427–39.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Eosinophilic Annular Erythema in a Patient with Eosinophilic Granulomatosis with Polyangiitis (Churg-Strauss Syndrome)
- Posttraumatic Guillain-Barré Syndrome Immediately Following a Traffic Accident
- A pediatric case of eosinophilic granulomatosis with polyangiitis accompanied by heart failure mimicking an asthma attack
- Eosinophilic Granulomatosis with Polyangiitis Presented as Acute Polyneuropathy and Cerebral Vasculitis
- Current Concept of Guillain-Barré Syndrome