Ann Surg Treat Res.
2018 Feb;94(2):106-111. 10.4174/astr.2018.94.2.106.
Single incision laparoscopic cholecystectomy for patients with Mirizzi syndrome
- Affiliations
-
- 1Department of Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. choiyoungrok@gmail.com
- KMID: 2402854
- DOI: http://doi.org/10.4174/astr.2018.94.2.106
Abstract
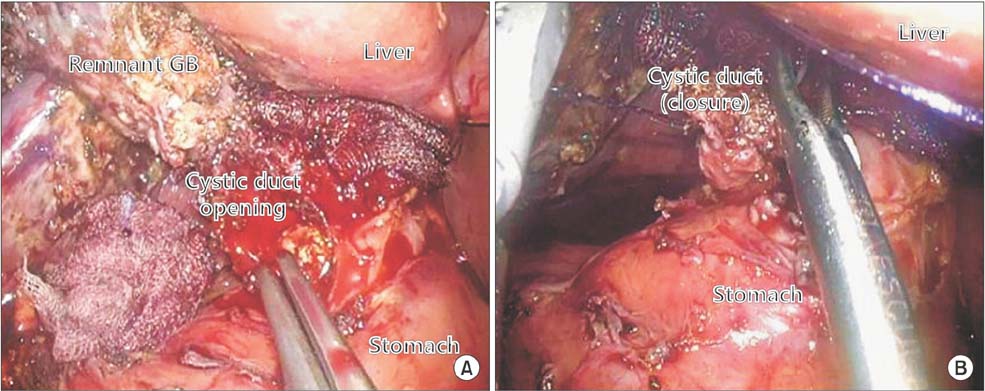
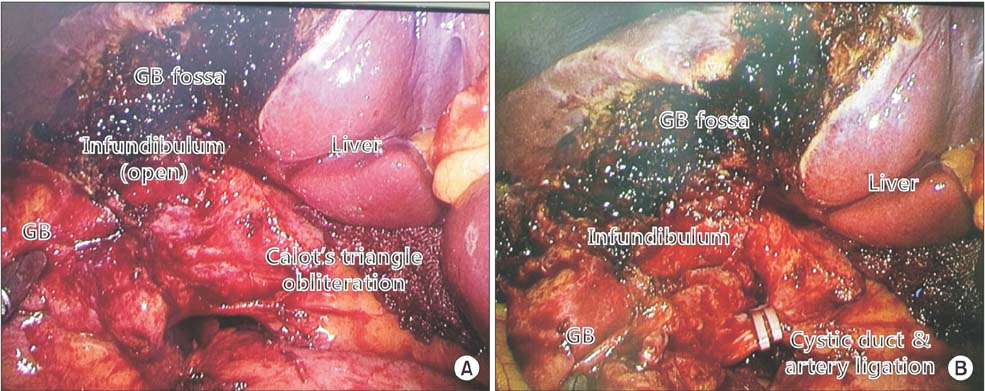
- Since multiport laparoscopic cholecystectomy has become a standard treatment for gallbladder (GB) disease, a single incision laparoscopic surgical technique has been tried to decrease the surgical site pain and achieve a better cosmetic out come in selected patients. The development of devices dedicated for single incision laparoscopic cholecystectomy (SILC) is expanding the indication of this single incision laparoscopic technique to more complicated GB diseases. Mirizzi syndrome (MS) is one of the complex uncommon gallstone diseases in patients undergoing cholecystectomy. Because the laparoscopic procedure has become a routine treatment for cholecystectomy, several studies have reported their experience with the laparoscopic technique for the treatment of MS with a comparable outcome in Csendes type I or II. Because the indication for SILC cholecystectomy is expanded to more complicated GB conditions, and the desire of patients for a less painful, better cosmetic surgical outcome has increased, our medical center used this single incision laparoscopic surgical technique for MS Csendes types I and II patients. Here, we report 2 successful cases of SILC for patients with MS types I and II without significant morbidity.
MeSH Terms
Figure
Reference
-
1. Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. One-wound laparoscopic cholecystectomy. Br J Surg. 1997; 84:695.
Article2. Philipp SR, Miedema BW, Thaler K. Single-incision laparoscopic cholecystectomy using conventional instruments: early experience in comparison with the gold standard. J Am Coll Surg. 2009; 209:632–637.
Article3. Ikumoto T, Yamagishi H, Iwatate M, Sano Y, Kotaka M, Imai Y. Feasibility of single-incision laparoscopic cholecystectomy for acute cholecystitis. World J Gastrointest Endosc. 2015; 7:1327–1333.
Article4. McSherry CK, Ferstenberg H, Virshup M. The Mirizzi syndrome: surggested classification and surgical therapy. Surg Gastroentrol. 1982; 1:219–225.5. Csendes A, Diaz JC, Burdiles P, Maluenda F, Nava O. Mirizzi syndrome and cholecystobiliary fistula: a unifying classification. Br J Surg. 1989; 76:1139–1143.
Article6. Rust KR, Clancy TV, Warren G, Mertesdorf J, Maxwell JG. Mirizzi's syndrome: a contraindication to coelioscopic cholecystectomy. J Laparoendosc Surg. 1991; 1:133–137.
Article7. Paul MG, Burris DG, McGuire AM, Thorfinnson HD, Schonekas H. Laparoscopic surgery in the treatment of Mirizzi's syndrome. J Laparoendosc Surg. 1992; 2:157–163.
Article8. Piccinni G, Sciusco A, De Luca GM, Gurrado A, Pasculli A, Testini M. Minimally invasive treatment of Mirizzi's syndrome: is there a safe way? Report of a case series. Ann Hepatol. 2014; 13:558–564.
Article9. Lledo JB, Barber SM, Ibanez JC, Torregrosa AG, Lopez-Andujar R. Update on the diagnosis and treatment of mirizzi syndrome in laparoscopic era: our experience in 7 years. Surg Laparosc Endosc Percutan Tech. 2014; 24:495–501.10. Ito M, Asano Y, Horiguchi A, Shimizu T, Yamamoto T, Uyama I, et al. Cholecystectomy using single-incision laparoscopic surgery with a new SILS port. J Hepatobiliary Pancreat Sci. 2010; 17:688–691.
Article11. Tam YH, Pang KK, Tsui SY, Wong YS, Wong HY, Mou JW, et al. Laparoendoscopic single-site nephrectomy and heminephroureterectomy in children using standard laparoscopic setup versus conventional laparoscopy. Urology. 2013; 82:430–435.
Article12. Kalteis M, Pistrich R, Schimetta W, Polz W. Laparoscopic cholecystectomy as solo surgery with the aid of a robotic camera holder: a case-control study. Surg Laparosc Endosc Percutan Tech. 2007; 17:277–282.13. Krajinovic K, Koeberlein C, Germer CT, Reibetanz J. The incidence of trocar site hernia after single-port laparoscopic chole cystectomy-a single center analysis and literature review. J Laparoendosc Adv Surg Tech A. 2016; 26:536–539.14. Arezzo A, Scozzari G, Famiglietti F, Passera R, Morino M. Is single-incision laparoscopic cholecystectomy safe? Results of a systematic review and meta-analysis. Surg Endosc. 2013; 27:2293–2304.
Article15. Yamashita Y, Takada T, Strasberg SM, Pitt HA, Gouma DJ, Garden OJ, et al. TG13 surgical management of acute cholecystitis. J Hepatobiliary Pancreat Sci. 2013; 20:89–96.16. Antoniou SA, Antoniou GA, Makridis C. Laparoscopic treatment of Mirizzi syndrome: a systematic review. Surg Endosc. 2010; 24:33–39.
Article17. Beltran MA. Mirizzi syndrome: history, current knowledge and proposal of a simplified classification. World J Gastroenterol. 2012; 18:4639–4650.18. Sare M, Gurer S, Taskin V, Aladag M, Hilmioglu F, Gurel M. Mirizzi syndrome: choice of surgical procedure in the laparoscopic era. Surg Laparosc Endosc. 1998; 8:63–67.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic management of Mirizzi syndrome with liver cirrhosis using indocyanine green mapping: A case report and review of the literature
- Laparoscopic treatment for post-cholecystectomy Mirizzi syndrome
- Mirizzi Syndrome: A Single Center Experience
- Comparison of Single-Incision Robotic Cholecystectomy, Single-Incision Laparoscopic Cholecystectomy and 3-Port Laparoscopic Cholecystectomy -Postoperative Pain, Cosmetic Outcome and Surgeon's Workload
- Minimally Invasive Approach Using Digital Single-Operator Peroral Cholangioscopy-Guided Electrohydraulic Lithotripsy and Endoscopic Nasogallbladder Drainage for the Management of High-Grade Mirizzi Syndrome