J Korean Soc Spine Surg.
2017 Mar;24(1):7-15. 10.4184/jkss.2017.24.1.7.
Conservative Treatment of Pyogenic Spondylitis in the Elderly
- Affiliations
-
- 1Department of Orthopedic Surgery, Gyeongsang National University School of Medicine, Jinju, Korea. ssurgeon@gnu.ac.kr
- 2Department of Orthopedic Surgery, Gyeongsang National University Changwon Hospital, Changwon, Korea.
- KMID: 2402837
- DOI: http://doi.org/10.4184/jkss.2017.24.1.7
Abstract
- STUDY DESIGN: Retrospective study.
OBJECTIVES
To analyze the outcomes of conservative management in elderly patients over 65 years of age who were diagnosed with pyogenic spondylitis. SUMMARY OF LITERATURE REVIEW: The surgical treatment of pyogenic spondylitis can lead to complications in elderly patients in a poor general condition or with underlying diseases.
MATERIALS AND METHODS
We performed a retrospective review of 32 patients who were diagnosed with pyogenic spondylitis and had a minimum of 12 months of follow-up. Age, sex, comorbidities, clinical symptoms, and the involved segments were analyzed retrospectively. The diagnosis was assessed using clinical, laboratory, and radiologic findings. Antibiotic therapy was either specific (if positive culture results were found) or broad-spectrum cephalosporin (when the pathogenic agent was not isolated). Outcomes were assessed using residual pain and neurologic deficits.
RESULTS
The mean onset time was 23.5 days (range, 3-90 days). The mean period of intravenous antibiotic therapy was 36.3 days (range, 10-90 days). All cases underwent conservative management, and 4 patients with progressive neurologic deficits due to epidural abscess underwent posterior laminectomy and abscess drainage. In all cases, the infection was successfully treated, although 12 cases reported residual lower back pain and 2 continued to exhibit minor neurologic deficits.
CONCLUSIONS
In elderly patients with pyogenic spondylitis, satisfactory results were obtained with conservative management using antibiotics and orthosis after an early diagnosis, unless progressive neurologic symptom instability or spine deformities were noted.
Keyword
MeSH Terms
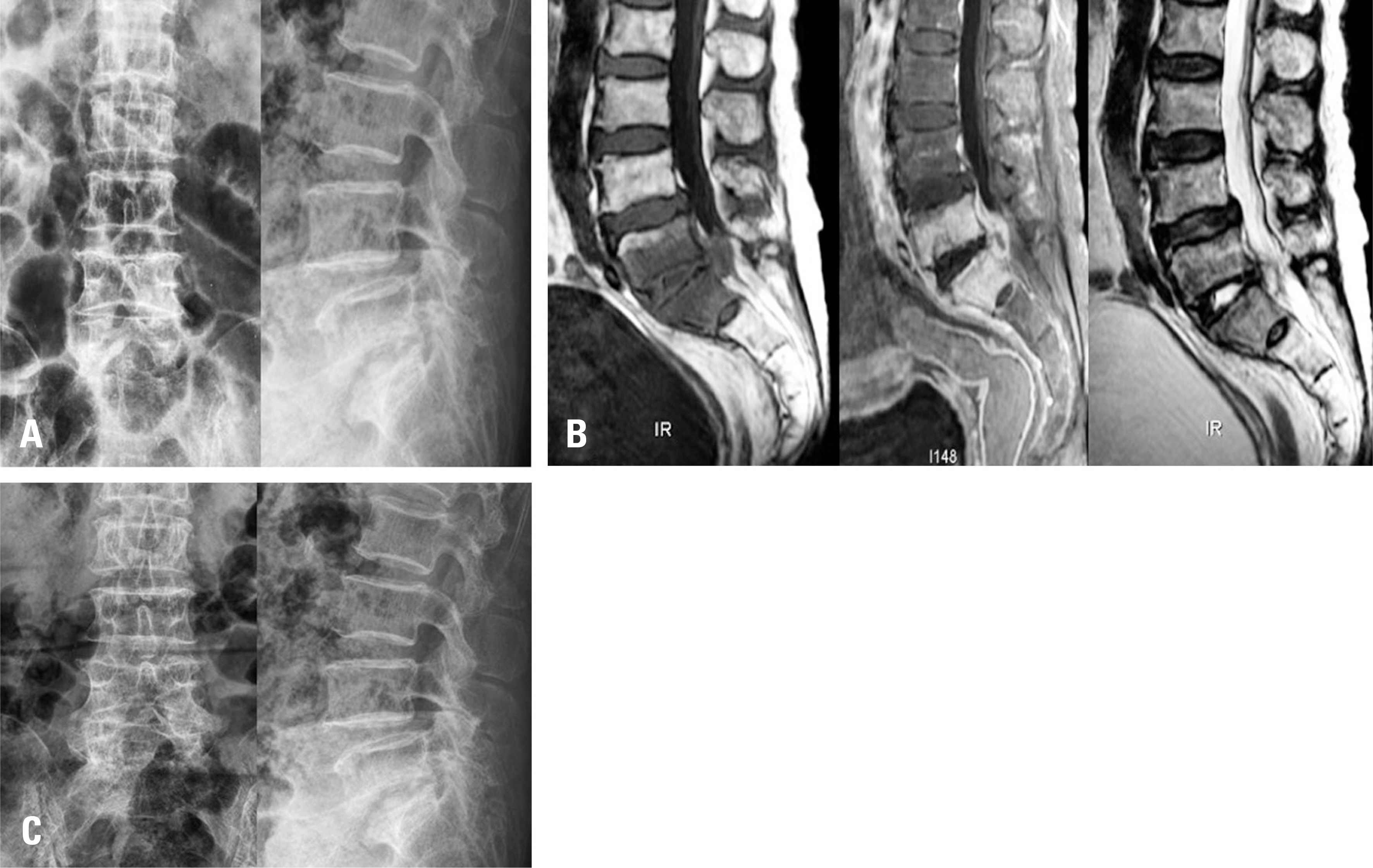
Figure
Cited by 1 articles
-
Comparison of the Results between Conservative and Operative Treatments for Pyogenic Spondylitis
Chang-Hwa Hong, Sangwoo Lee, Woo-Jong Kim, Jaewan Soh
J Korean Orthop Assoc. 2018;53(4):332-340. doi: 10.4055/jkoa.2018.53.4.332.
Reference
-
1. Skaf GS, Domloj NT, Fehlings MG, et al. Pyogenic spondylodiscitis: an overview. J Infect Public Health. 2010; 3:5–16.
Article2. Govender S. Spinal infections. J Bone Joint Surg Br. 2005; 87:1454–8.
Article3. Lestini WF, Fulghum JS, Whitehurst LA. Lumbar spinal fusion: advantages of posterior lumbar interbody fusion. Surg Technol Int. 1994; 3:577–90.4. Torda AJ, Gottlieb T, Bradbury R. Pyogenic vertebral osteomyelitis: analysis of 20 cases and review. Clin Infect Dis. 1995; 20:320–8.
Article5. Thelander U, Larsson S. Quantitation of C-reactive protein levels and erythrocyte sedimentation rate after spinal surgery. Spine (Phila Pa 1976). 1992; 17:400–4.
Article6. Yoshimoto M, Takebayashi T, Kawaguchi S, et al. Pyogenic spondylitis in the elderly: a report from Japan with the most aging society. Eur Spine J. 2011; 20:649–54.
Article7. Bettini N, Girardo M, Dema E, et al. Evaluation of conservative treatment of non specific spondylodiscitis. Eur Spine J. 2009; 18(Suppl):143–50.
Article8. Butler JS, Shelly MJ, Timlin M, et al. Nontuberculous pyogenic spinal infection in adults: a 12-year experi-ence from a tertiary referral center. Spine (Phila Pa 1976). 2006; 31:2695–700.9. Ozuna RM, Delamarter RB. Pyogenic vertebral osteomyelitis and postsurgical disc space infections. Orthop Clin North Am. 1996; 27:87–94.
Article10. Buranapanitkit B, Lim A, Kiriratnikom T. Clinical manifes-tation of tuberculous and pyogenic spine infection. J Med Assoc Thai. 2001; 84:1522–6.11. Mylona E, Samarkos M, Kakalou E, et al. Pyogenic vertebral osteomyelitis: a systematic review of clinical character-istics. Semin Arthritis Rheum. 2009; 39:10–7.
Article12. Oostveen JC, van de Laar MA. Magnetic resonance imaging in rheumatic disorders of the spine and sacroiliac joints. Semin Arthritis Rheum. 2000; 30:52–69.
Article13. Carragee EJ. Pyogenic vertebral osteomyelitis. J Bone Joint Surg Am. 1997; 79:874–80.
Article14. Dagirmanjian A, Schils J, McHenry MC. MR imaging of spinal infections. Magn Reson Imaging Clin N Am. 1999; 7:525–38.
Article15. Sharif HS. Role of MR imaging in the management of spinal infections. AJR Am J Roentgenol. 1992; 158:1333–45.
Article16. Luzzati R, Giacomazzi D, Danzi MC, et al. Diagnosis, management and outcome of clinically- suspected spinal infection. J Infect. 2009; 58:259–65.
Article17. Grados F, Lescure FX, Senneville E, et al. Suggestions for managing pyogenic (nontuberculous) discitis in adults. Joint Bone Spine. 2007; 74:133–9.
Article18. Hadjipavlou AG, Katonis PK, Gaitanis IN, et al. Percutaneous transpedicular discectomy and drainage in pyogenic spondylodiscitis. Eur Spine J. 2004; 13:707–13.
Article19. Rath SA, Neff U, Schneider O, et al. Neurosurgical management of thoracic and lumbar vertebral osteomyelitis and discitis in adults: a review of 43 consecutive surgically treated patients. Neurosurgery. 1996; 38:926–33.
Article20. Roblot F, Besnier JM, Juhel L, et al. Optimal duration of antibiotic therapy in vertebral osteomyelitis. Semin Arthritis Rheum. 2007; 36:269–77.
Article21. Sapico FL. Microbiology and antimicrobial therapy of spinal infections. Orthop Clin North Am. 1996; 27:9–13.
Article22. Eismont FJ, Bohlman HH, Soni PL, et al. Pyogenic and fungal vertebral osteomyelitis with paralysis. J Bone Joint Surg Am. 1983; 65:19–29.
Article23. Perronne C, Saba J, Behloul Z, et al. Pyogenic and tuberculous spondylodiskitis (vertebral osteomyelitis) in 80 adult patients. Clin Infect Dis. 1994; 19:746–50.
Article24. Tsiodras S, Falagas ME. Clinical assessment and medical treatment of spine infections. Clin Orthop Relat Res. 2006; 444:38–50.
Article25. Acosta FL Jr., Galvez LF, Aryan HE, et al. Recent advanc-es: infections of the spine. Curr Infect Dis Rep. 2006; 8:390–3.
Article26. Quinones-Hinojosa A, Jun P, Jacobs R, et al. General principles in the medical and surgical management of spinal infections: a multidisciplinary approach. Neurosurg Focus. 2004; 17:E1.27. Pigrau C, Almirante B, Flores X, et al. Spontaneous pyogenic vertebral osteomyelitis and endocarditis: incidence, risk factors, and outcome. Am J Med. 2005; 118:1287.
Article28. Park W-W, Park Y-S, Cheon S-J, et al. Posterior lumbar interbody fusion in the pyogenic discitis. J Korean Soc Spine Surg. 2001; 8:39–45.
Article29. Shin D-E, Kim H-S, Ahn C-S, et al. Anterior debridement and strut graft with pedicle screw fixation for pyogenic spondylitis. Asian Spine J. 2007; 1:91–7.
Article30. Cho B-K, Kim Y-M, Kim D-S, et al. Management of lumbar pyogenic spondylitis with posterior decompression and interbody fusion using transpedicular screws. J Korean Orthop Assoc. 2010; 45:165–72.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Pyogenic Spondylitis and Tuberculous Spondylitis
- 3 Cases of Pyogenic spondylitis
- Comparison of the Results between Conservative and Operative Treatments for Pyogenic Spondylitis
- Streptococcus Spondylitis Concomitant Infectious Endocarditis: A Case Report
- Comparison of Pyogenic and Tuberculous Spondylitis