Korean J Ophthalmol.
2018 Feb;32(1):65-69. 10.3341/kjo.2016.0092.
Fluorescein Angiographic Abnormalities in the Contralateral Eye with Normal Fundus in Children with Unilateral Coats' Disease
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea. ysyu@snu.ac.kr
- 2Seoul Artificial Eye Center, Seoul National University Hospital Clinical Research Institute, Seoul, Korea.
- KMID: 2402722
- DOI: http://doi.org/10.3341/kjo.2016.0092
Abstract
- PURPOSE
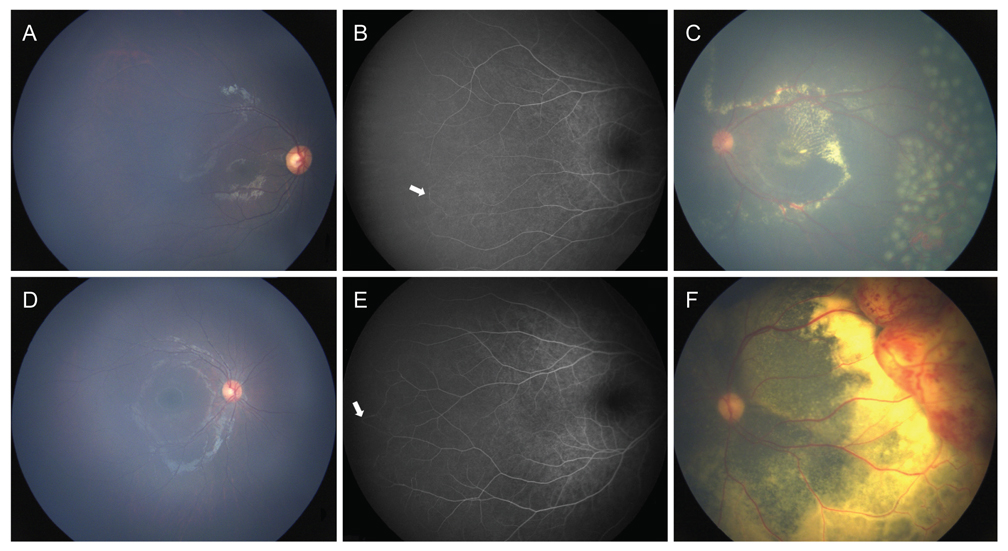
We report the detection of peripheral retinal vascular abnormalities in the fellow eye with normal fundus in children with unilateral Coats' disease.
METHODS
The clinical records of patients diagnosed with Coats' disease were retrospectively reviewed. We recorded the subjects' characteristics and obtained fundus photography and fluorescein angiography (FA) images. The main outcome measure was peripheral vascular abnormalities in the contralateral eye with normal fundus in children with unilateral Coats' disease, observed with FA.
RESULTS
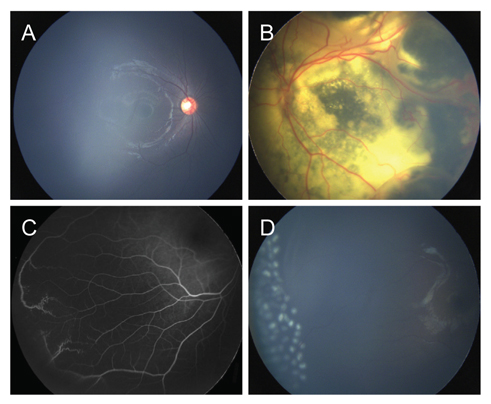
Out of 47 patients with Coats' disease, two (4.3%) were diagnosed with clinically bilateral Coats' disease. Of the 45 patients with presumed unilateral Coats' disease, four (8.9%) had bilateral abnormal peripheral vasculature in FA. The mean age of these four patients was 6.4 ± 5.4 years (range, 1 to 14 years), and three patients were male (75%). All four had peripheral retinal nonperfusion, and two (50%) received laser photocoagulation due to peripheral leakage with telangiectatic vessels.
CONCLUSIONS
Coats' disease may more often be a bilateral disease with asymmetry than previously thought. Patients with Coats' disease should undergo careful examination of the fellow eye with FA in order to detect and treat vascular abnormalities that are not visible clinically.
MeSH Terms
Figure
Reference
-
1. Shields JA, Shields CL, Honavar SG, Demirci H. Clinical variations and complications of Coats disease in 150 cases: the 2000 Sanford Gifford Memorial Lecture. Am J Ophthalmol. 2001; 131:561–571.
Article2. Woods AC, Duke JR. Coats's disease. I. Review of the literature, diagnostic criteria, clinical findings, and plasma lipid studies. Br J Ophthalmol. 1963; 47:385–412.
Article3. Egerer I, Tasman W, Tomer TT. Coats disease. Arch Ophthalmol. 1974; 92:109–112.
Article4. Spitznas M, Joussen F, Wessing A, Meyer-Schwickerath G. Coat's disease: an epidemiologic and fluorescein angiographic study. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1975; 195:241–250.5. Tarkkanen A, Laatikainen L. Coat's disease: clinical, angiographic, histopathological findings and clinical management. Br J Ophthalmol. 1983; 67:766–776.
Article6. Shienbaum G, Tasman WS. Coats disease: a lifetime disease. Retina. 2006; 26:422–424.7. Rishi P, Rishi E, Uparkar M, et al. Coats' disease: an Indian perspective. Indian J Ophthalmol. 2010; 58:119–124.
Article8. Suzani M, Moore AT. Intraoperative fluorescein angiography-guided treatment in children with early Coats' disease. Ophthalmology. 2015; 122:1195–1202.
Article9. Blair MP, Ulrich JN, Elizabeth Hartnett M, Shapiro MJ. Peripheral retinal nonperfusion in fellow eyes in coats disease. Retina. 2013; 33:1694–1699.
Article10. Shane TS, Berrocal AM, Hess DJ. Bilateral fluorescein angiographic findings in unilateral Coats' disease. Ophthalmic Surg Lasers Imaging. 2011; 42:e15–e17.
Article11. Blair MP, Shapiro MJ, Hartnett ME. Fluorescein angiography to estimate normal peripheral retinal nonperfusion in children. J AAPOS. 2012; 16:234–237.
Article12. Ghorbanian S, Jaulim A, Chatziralli IP. Diagnosis and treatment of coats' disease: a review of the literature. Ophthalmologica. 2012; 227:175–182.
Article13. Shields JA, Shields CL, Honavar SG, et al. Classification and management of Coats disease: the 2000 Proctor Lecture. Am J Ophthalmol. 2001; 131:572–583.
Article14. Rutnin U, Schepens CL. Fundus appearance in normal eyes. II. The standard peripheral fundus and developmental variations. Am J Ophthalmol. 1967; 64:840–852.15. Rutnin U, Schepens CL. Fundus appearance in normal eyes. IV. Retinal breaks and other findings. Am J Ophthalmol. 1967; 64:1063–1078.16. Rutnin U, Schepens CL. Fundus appearance in normal eyes. 3. Peripheral degenerations. Am J Ophthalmol. 1967; 64:1040–1062.17. Lai CH, Kuo HK, Wu PC, et al. Manifestation of Coats' disease by age in Taiwan. Clin Exp Ophthalmol. 2007; 35:361–365.
Article18. Sims KB. NDP-related retinopathies. In : Pagon RA, Adam MP, Ardinger HH, editors. GeneReviews(R). Seattle: University of Washington;2014.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Retinoblastoma and Coats' Disease in the Same eye: A Clinicopathologic Report
- Bilateral Fundus Findings Using Examination Under Anesthesia in Patients Showing Vitreoretinopathy at Unilateral Posterior Pole
- A Case of Coats' Disease Accompanying A Retinal Macrocyst
- Bilateral Coats' Disease: A Case Report
- Combined Photodynamic Therapy and Intravitreal Bevacizumab Injection for the Treatment of Adult Coats' Disease: A Case Report