Intest Res.
2018 Jan;16(1):69-74. 10.5217/ir.2018.16.1.69.
Are Truelove and Witts criteria for diagnosing acute severe colitis relevant for the Indian population? A prospective study
- Affiliations
-
- 1Department of Gastroenterology, All India Institute of Medical Sciences, New Delhi, India. vineet.aiims@gmail.com
- 2Department of Gastrointestinal Surgery, All India Institute of Medical Sciences, New Delhi, India.
- 3Translational Gastroenterology Unit, Oxford University Hospitals, Oxford, UK.
- KMID: 2402649
- DOI: http://doi.org/10.5217/ir.2018.16.1.69
Abstract
- BACKGROUND/AIMS
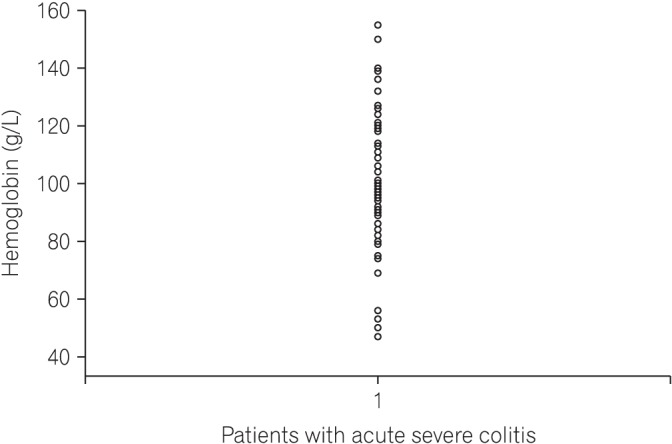
Truelove and Witts criteria have been used to define acute severe colitis since the 1950s. However, hemoglobin (an additional criterion of the definition) levels in the general population in developing countries are lower than in the population of developed countries. We aimed to determine the relevance of Truelove and Witts criteria in the Indian population.
METHODS
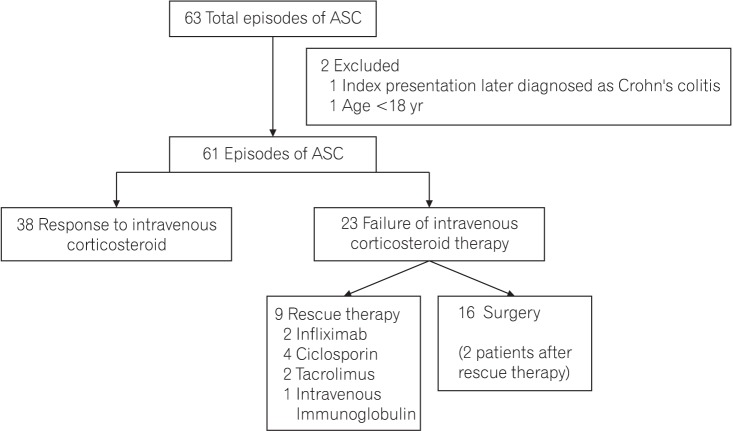
Consecutive patients with acute severe colitis satisfying the Truelove and Witts criteria, hospitalized at a single center between April 2015 and December 2016 were included. All patients received intravenous corticosteroids and 16 required colectomy. The hemoglobin levels at admission were subsequently excluded from the classification criteria, and the effect this had on the criteria for diagnosis was determined.
RESULTS
Out of 61 patients of acute severe colitis diagnosed according to the original Truelove and Witts criteria, 12 patients (20%) had 1 additional criterion, 33 (54%) had 2 additional criteria and 16 (26%) had 3 or more additional criteria in addition to 6 or more blood stained stools on admission. On excluding hemoglobin as an additional criterion from the Truelove and Witts definition, all patients still met the criteria for acute severe colitis.
CONCLUSIONS
Truelove and Witts criteria can be used to define acute severe colitis in India, despite lower mean hemoglobin in the native population.
MeSH Terms
Figure
Reference
-
1. Singh P, Ananthakrishnan A, Ahuja V. Pivot to Asia: inflammatory bowel disease burden. Intest Res. 2017; 15:138–141. PMID: 28239326.
Article2. Kedia S, Ahuja V. Epidemiology of inflammatory bowel disease in India: the Great Shift East [published online ahead of print April 18, 2017]. Inflamm Intest Dis. DOI: 10.1159/000465522.3. Ng WK, Wong SH, Ng SC. Changing epidemiological trends of inflammatory bowel disease in Asia. Intest Res. 2016; 14:111–119. PMID: 27175111.
Article4. Dinesen LC, Walsh AJ, Protic MN, et al. The pattern and outcome of acute severe colitis. J Crohns Colitis. 2010; 4:431–437. PMID: 21122540.
Article5. Edwards FC, Truelove SC. The course and prognosis of ulcerative colitis. Gut. 1963; 4:299–315. PMID: 14084741.6. Jain S, Kedia S, Bopanna S, et al. Faecal calprotectin and UCEIS predict short-term outcomes in acute severe colitis: prospective cohort study. J Crohns Colitis. 2017; 11:1309–1316. PMID: 29088461.
Article7. Truelove SC, Witts LJ. Cortisone in ulcerative colitis; preliminary report on a therapeutic trial. Br Med J. 1954; 2:375–378. PMID: 13182220.
Article8. Magro F, Gionchetti P, Eliakim R, et al. Third European evidence-based consensus on diagnosis and management of ulcerative colitis. Part 1: definitions, diagnosis, extra-intestinal manifestations, pregnancy, cancer surveillance, surgery, and ileo-anal pouch disorders. J Crohns Colitis. 2017; 11:649–670. PMID: 28158501.
Article9. Kornbluth A, Sachar DB. Practice Parameters Committee of the American College of Gastroenterology. Ulcerative colitis practice guidelines in adults: American College Of Gastroenterology, Practice Parameters Committee. Am J Gastroenterol. 2010; 105:501–523. PMID: 20068560.
Article10. Mowat C, Cole A, Windsor A, et al. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2011; 60:571–607. PMID: 21464096.
Article11. Brown SR, Haboubi N, Hampton J, George B, Travis SP. ACPGBI. The management of acute severe colitis: ACPGBI position statement. Colorectal Dis. 2008; 10(Suppl 3):8–29. PMID: 18954307.
Article12. Nutritional anaemias: report of a WHO scientific group. World Health Organ Tech Rep Ser. 1968; 405:5–37. PMID: 4975372.13. Yip R. Final report of the 1995 Viet Nam National Nutrition Anemia and Intestinal Helminth Survey: a recommended plan of action for the control of iron deficiency for Viet Nam. Jakarta: United Nations Children's Fund Indonesia;1996.14. Ashavaid TF, Todur SP, Dherai AJ. Establishment of reference intervals in Indian population. Indian J Clin Biochem. 2005; 20:110–118. PMID: 23105542.
Article15. Dignass A, Eliakim R, Magro F, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 1: definitions and diagnosis. J Crohns Colitis. 2012; 6:965–990. PMID: 23040452.
Article16. Silverberg MS, Satsangi J, Ahmad T, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005; 19(Suppl A):5A–36A.
Article17. Travis SP, Schnell D, Krzeski P, et al. Reliability and initial validation of the ulcerative colitis endoscopic index of severity. Gastroenterology. 2013; 145:987–995. PMID: 23891974.
Article18. Dignass A, Lindsay JO, Sturm A, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 2: current management. J Crohns Colitis. 2012; 6:991–1030. PMID: 23040451.
Article19. Travis SP, Farrant JM, Ricketts C, et al. Predicting outcome in severe ulcerative colitis. Gut. 1996; 38:905–910. PMID: 8984031.
Article20. Merkley SA, Beaulieu DB, Horst S, et al. Use of intravenous immunoglobulin for patients with inflammatory bowel disease with contraindications or who are unresponsive to conventional treatments. Inflamm Bowel Dis. 2015; 21:1854–1859. PMID: 25993689.
Article21. Levine DS, Fischer SH, Christie DL, Haggitt RC, Ochs HD. Intravenous immunoglobulin therapy for active, extensive, and medically refractory idiopathic ulcerative or Crohn's colitis. Am J Gastroenterol. 1992; 87:91–100. PMID: 1728132.22. Llaó J, Naves JE, Ruiz-Cerulla A, et al. Improved outcome of acute severe ulcerative colitis while using early predictors of corticosteroid failure and rescue therapies. Dig Liver Dis. 2016; 48:608–612. PMID: 27012443.
Article23. Ho GT, Mowat C, Goddard CJ, et al. Predicting the outcome of severe ulcerative colitis: development of a novel risk score to aid early selection of patients for second-line medical therapy or surgery. Aliment Pharmacol Ther. 2004; 19:1079–1087. PMID: 15142197.
Article24. Corte C, Fernandopulle N, Catuneanu AM, et al. Association between the ulcerative colitis endoscopic index of severity (UCEIS) and outcomes in acute severe ulcerative colitis. J Crohns Colitis. 2015; 9:376–381. PMID: 25770163.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Chronological Review of Endoscopic Indices in Inflammatory Bowel Disease
- High mucosal cytomegalovirus DNA helps predict adverse short-term outcome in acute severe ulcerative colitis
- Red Cell Distribution Width: A Novel Marker of Activity in Inflammatory Bowel Disease
- A Case of Acute Pancreatitis associated with Ulcerative Colitis
- Comparative Usefulness of Erythrocyte Sedimentation Rate and C-reactive Protein in Assessing the Severity of Ulcerative Colitis