J Korean Ophthalmol Soc.
2018 Jan;59(1):81-86. 10.3341/jkos.2018.59.1.81.
Optic Neuritis of Korean Adult
- Affiliations
-
- 1Department of Ophthalmology, Chungnam National University School of Medicine, Daejeon, Korea. opticalyh@hanmail.net
- KMID: 2401682
- DOI: http://doi.org/10.3341/jkos.2018.59.1.81
Abstract
- PURPOSE
The aim of the study was to describe the clinical features and characteristics of optic neuritis patients compared with those of patients enrolled in the Optic Neuritis Treatment Trial (ONTT).
METHODS
We retrospectively included consecutive patients diagnosed with optic neuritis between 2006 and 2015. The inclusion criteria were the same as those of the ONTT; an acute or subacute unilateral visual symptom ≤8 days in duration, a relative afferent pupillary defect, and a visual field defect in the affected eye.
RESULTS
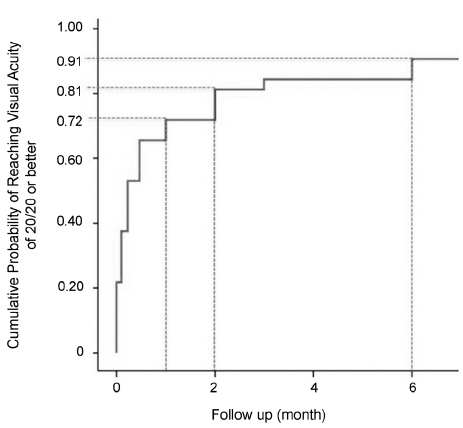
The 41 patients (14 females, 27 males) were of mean age 32.7 years. The incidence of papilledema was 58.5%, thus higher than that of ONTT patients (p = 0.004), and the incidence of ocular pain was 75.6%, lower than that of ONTT patients (p = 0.002). Six months after intravenous methylprednisolone therapy, 29 of 32 eyes (90.6%) recovered visual acuity of ≥1.0 or better, and only one eye exhibited poor visual acuity (≤0.5). Orbital magnetic resonance imaging (MRI) was performed on 34 patients, and most (91.2%) exhibited optic nerve enhancement. The three patients who did not exhibit enhancement reported no pain.
CONCLUSIONS
The clinical features of Korean optic neuritis patients differed from those of patients of the ONTT. Most patients exhibited optic nerve MRI enhancement associated with ocular pain. If enhancement of the optic nerve is lacking, diseases other than optic neuritis should be suspected because most optic nerves with neuritis exhibit enhancement on MRI.
MeSH Terms
Figure
Reference
-
1. Hickman SJ, Miszkiel KA, Plant GT, Miller DH. The optic nerve sheath on MRI in acute optic neuritis. Neuroradiology. 2005; 47:51–55.
Article2. Hickman SJ, Dalton CM, Miller DH, Plant GT. Management of acute optic neuritis. Lancet. 2002; 360:1953–1962.
Article3. Optic Neuritis Study Group. Visual function 15 years after optic neuritis: a final follow-up report from the Optic Neuritis Treatment Trial. Ophthalmology. 2008; 115:1079–1082.4. Beck RW, Gal RL, Bhatti MT, et al. Visual function more than 10 years after optic neuritis: experience of the optic neuritis treatment trial. Am J Ophthalmol. 2004; 137:77–83.5. Optic Neuritis Study Group. The clinical profile of optic neuritis. Experience of the Optic Neuritis Treatment Trial. Arch Ophthalmol. 1991; 109:1673–1678.6. Beck RW, Cleary PA, Anderson MM Jr, et al. A randomized, controlled trial of corticosteroids in the treatment of acute optic neuritis. The Optic Neuritis Study Group. N Engl J Med. 1992; 326:581–588.7. Volpe NJ. The optic neuritis treatment trial: a definitive answer and profound impact with unexpected results. Arch Ophthalmol. 2008; 126:996–999.8. Lee YJ, Kim MK, Hwang JM. Optic neuritis in Children. J Korean Ophthalmol Soc. 2002; 43:314–319.9. Choi MY, Hwang JM. Clinical characteristics of optic neuritis associated with multiple sclerosis. J Korean Ophthalmol Soc. 2000; 41:1216–1223.10. Ahn BC, Kim HS, Ahn HS. Clinical profile of the optic neuritis in Korea. J Korean Ophthalmol Soc. 1997; 38:1827–1833.11. Cha DM, Kim SJ, Kim JH, et al. Clinical features and the effect of high-dose steroid therapy in Korean optic neuritis patients. J Korean Ophthalmol Soc. 2011; 52:1083–1088.
Article12. Kang HM, Kim HY. Clinical manifestations of idiopathic optic perineuritis in Korea. J Korean Ophthalmol Soc. 2012; 53:1016–1022.
Article13. Beck RW, Cleary PA. Optic neuritis treatment trial. One-year follow-up results. Arch Ophthalmol. 1993; 111:773–775.14. Pau D, Al Zubidi N, Yalamanchili S, et al. Optic neuritis. Eye (Lond). 2011; 25:833–842.
Article15. Warren S, Warren KG. Prevalence of multiple sclerosis in Barrhead County, Alberta, Canada. Can J Neurol Sci. 1992; 19:72–75.
Article16. Comi G, Filippi M, Barkhof F, et al. Effect of early interferon treatment on conversion to definite multiple sclerosis: a randomised study. Lancet. 2001; 357:1576–1582.
Article17. Sandberg-Wollheim M, Bynke H, Cronqvist S, et al. A long-term prospective study of optic neuritis: evaluation of risk factors. Ann Neurol. 1990; 27:386–393.
Article18. Lim HC, Choi HY, Choi JH, Jung JH. Clinical manifestations and treatment of idiopathic optic perineuritis. J Korean Ophthalmol Soc. 2014; 55:891–897.
Article19. Lim SA, Goh KY, Tow S, et al. Optic neuritis in Singapore. Singapore Med J. 2008; 49:667–671.20. Wakakura M, Minei-Higa R, Oono S, et al. Optic Neuritis Treatment Trial Multicenter Cooperative Research Group (ONMRG). Baseline features of idiopathic optic neuritis as determined by a multicenter treatment trial in Japan. Jpn J Ophthalmol. 1999; 43:127–132.
Article21. Wang JC, Tow S, Aung T, et al. The presentation, aetiology, management and outcome of optic neuritis in an Asian population. Clin Exp Ophthalmol. 2001; 29:312–315.
Article22. Kira J. Multiple sclerosis in the Japanese population. Lancet Neurology. 2003; 2:117–127.
Article23. Lin YC, Yen MY, Hsu WM, et al. Low conversion rate to multiple sclerosis in idiopathic optic neuritis patients in Taiwan. Jpn J Ophthalmol. 2006; 50:170–175.
Article24. Kim YM, Kim HY, Cho MJ, et al. Optic neuritis in Korean children: low risk of subsequent multiple sclerosis. Pediatr Neurol. 2015; 53:221–225.
Article25. Leibowitz U, Alter M, Halpern L. Clinical studies of multiple sclerosis in Israel. IV. Optic neuropathy and multiple sclerosis. Arch Neurol. 1966; 14:459–466.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Optic Disc Hamartoma Combined with Optic Neuritis
- A case of Crohn's Disease with Optic Neuritis and Wernicke's Encephalopathy
- Reversible Bilateral Optic Neuritis with No Light Perception
- Clinical Manifestations of Idiopathic Optic Perineuritis in Korea
- Possible Tuberculous Meningitis Complicated with Optic Neuritis