Pediatr Infect Vaccine.
2017 Aug;24(2):71-78. 10.14776/piv.2017.24.2.71.
Etiology of Bacteremia in Children with Hemato-oncologic Diseases from a Single Center from 2011 to 2015
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children's Hospital, Seoul National University College of Medicine, Seoul, the Republic of Korea. eunchoi@snu.ac.kr
- 2Department of Pediatrics, Seoul National University College of Medicine, Seoul, the Republic of Korea.
- KMID: 2401447
- DOI: http://doi.org/10.14776/piv.2017.24.2.71
Abstract
- PURPOSE
The aim of this study was to identify the pathogens of blood stream infection (BSI) in children with hemato-oncologic disorders, to analyze susceptibility patterns of microorganisms to guide empirical antimicrobial therapy, and to compare temporal trends of the pathogen and antimicrobial susceptibility with those of previous studies.
METHODS
We retrospectively analyzed the medical records of children with hemato-oncologic disorders whose blood culture grew pathogens at the Seoul National University Children's Hospital between 2011 and 2015.
RESULTS
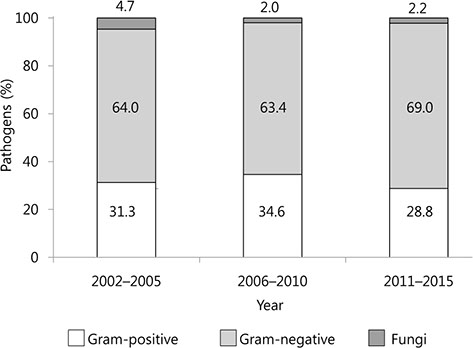
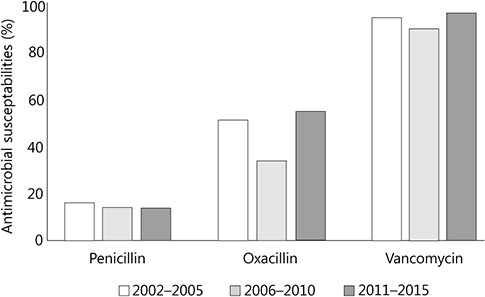
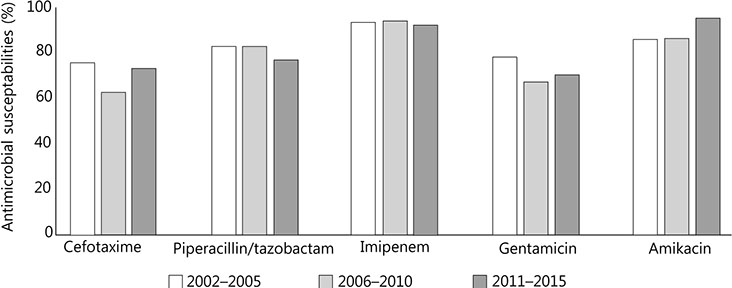
A total of 167 patients developed 221 episodes of bacteremia. Among 229 pathogens, gram-negative bacteria (GNB) accounted for 69.0% (64.0% in 2002 to 2005, 63.4% in 2006 to 2010); gram-positive bacteria (GPB) accounted for 28.8% (31.3% in 2002 to 2005, 34.6% in 2006 to 2010); and fungus accounted for 2.2%. Among GNB, Klebsiella species (53.2%, 84/158) and Escherichia coli (19.6%, 31/158) were common. Staphylococcus aureus (48.5%, 32/66) and viridans streptococci (21.2%, 14/66) were frequently isolated among GPB. The susceptibilities of oxacillin and vancomycin in GPB were 54.8% and 96.9% (51.5% and 95.5% in 2002 to 2005; 34.1% and 90.5% in 2006 to 2010), respectively, whereas in GNB, the susceptibilities of cefotaxime, piperacillin/tazobactam, and imipenem were 73.2%, 77.2%, and 92.6% (75.9%, 82.8%, and 93.4% in 2002 to 2005; 62.8%, 82.9%, 93.8% and in 2006 to 2010), respectively. There were no significant differences in the proportion of etiologic agents or the antimicrobial susceptibilities between the current study and that of the previous two studies from 2002 to 2010. Overall fatality rate was 13.1%.
CONCLUSIONS
GNB predominated in BSI among children with hemato-oncologic disorders. The etiology of bacteremia and antimicrobial susceptibility were comparable to those of the previous studies. Thus, piperacillin/tazobactam can be used as the initial empirical antimicrobial agent in febrile neutropenia.
Keyword
MeSH Terms
Figure
Reference
-
1. Viscoli C, Varnier O, Machetti M. Infections in patients with febrile neutropenia: epidemiology, microbiology, and risk stratification. Clin Infect Dis. 2005; 40:Suppl 4. S240–S245.
Article2. Pizzo PA. Management of fever in patients with cancer and treatment-induced neutropenia. N Engl J Med. 1993; 328:1323–1332.
Article3. Klastersky J, Ameye L, Maertens J, Georgala A, Muanza F, Aoun M, et al. Bacteraemia in febrile neutropenic cancer patients. Int J Antimicrob Agents. 2007; 30:Suppl 1. S51–S59.
Article4. Norgaard M, Larsson H, Pedersen G, Schonheyder HC, Sorensen HT. Risk of bacteraemia and mortality in patients with haematological malignancies. Clin Microbiol Infect. 2006; 12:217–223.
Article5. Aust C, Tolfvenstam T, Broliden K, Ljungman P, Kalin M, Giske CG, et al. Bacteremia in Swedish hematological patients with febrile neutropenia: bacterial spectrum and antimicrobial resistance patterns. Scand J Infect Dis. 2013; 45:285–291.
Article6. Singer C, Kaplan MH, Armstrong D. Bacteremia and fungemia complicating neoplastic disease. A study of 364 cases. Am J Med. 1977; 62:731–742.7. Zinner SH. Changing epidemiology of infections in patients with neutropenia and cancer: emphasis on gram-positive and resistant bacteria. Clin Infect Dis. 1999; 29:490–494.
Article8. Wisplinghoff H, Seifert H, Wenzel RP, Edmond MB. Current trends in the epidemiology of nosocomial bloodstream infections in patients with hematological malignancies and solid neoplasms in hospitals in the United States. Clin Infect Dis. 2003; 36:1103–1110.
Article9. Ramphal R. Changes in the etiology of bacteremia in febrile neutropenic patients and the susceptibilities of the currently isolated pathogens. Clin Infect Dis. 2004; 39:Suppl 1. S25–S31.
Article10. Gudiol C, Bodro M, Simonetti A, Tubau F, Gonzalez-Barca E, Cisnal M, et al. Changing aetiology, clinical features, antimicrobial resistance, and outcomes of bloodstream infection in neutropenic cancer patients. Clin Microbiol Infect. 2013; 19:474–479.
Article11. Elting LS, Bodey GP, Keefe BH. Septicemia and shock syndrome due to viridans streptococci: a case-control study of predisposing factors. Clin Infect Dis. 1992; 14:1201–1207.
Article12. Cordonnier C, Buzyn A, Leverger G, Herbrecht R, Hunault M, Leclercq R, et al. Epidemiology and risk factors for gram-positive coccal infections in neutropenia: toward a more targeted antibiotic strategy. Clin Infect Dis. 2003; 36:149–158.
Article13. Kim SH, Lee YA, Eun BW, Kim NH, Lee JA, Kang HJ, et al. Etiological agents isolated from blood in children with hemato-oncologic diseases (2002–2005). Korean J Pediatr. 2007; 50:56–64.
Article14. Kang JE, Seok JY, Yun KW, Kang HJ, Choi EH, Park KD, et al. Etiological agents in bacteremia of children with hematooncologic diseases (2006–2010): a single center study. Korean J Pediatr Infect Dis. 2012; 19:131–140.
Article15. Mermel LA, Allon M, Bouza E, Craven DE, Flynn P, O'Grady NP, et al. Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2009; 49:1–45.
Article16. Kleinman ME, Chameides L, Schexnayder SM, Samson RA, Hazinski MF, Atkins DL, et al. Pediatric advanced life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Pediatrics. 2010; 126:e1361–e1399.
Article17. Maki DG, Mermel LA, Kluger D, Narans L, Knasinski V, Parenteau S, et al. The efficacy of a chlorhexidine-impregnated sponge (biopatch) for the prevention of intravascular catheter-related infection: a prospective, randomized, controlled, multicenter study. In : Present at the 40th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2000 Sep 17–20; Toronto, Canada.18. Levy I, Katz J, Solter E, Samra Z, Vidne B, Birk E, et al. Chlorhexidine-impregnated dressing for prevention of colonization of central venous catheters in infants and children: a randomized controlled study. Pediatr Infect Dis J. 2005; 24:676–679.
Article19. Ho KM, Litton E. Use of chlorhexidine-impregnated dressing to prevent vascular and epidural catheter colonization and infection: a meta-analysis. J Antimicrob Chemother. 2006; 58:281–287.
Article20. Rivas-Ruiz R, Villasis-Keever MA, Miranda-Novales MG, Castelan-Martinez D, Vivanco-Munoz N, Chico-Barba G, et al. Efficacy of a chlorhexidine-gluconate impregnated patch for prevention of catheter-related infections in pediatric patients: systematic review and meta-analysis. Bol Med Hosp Infant Mex. 2011; 68:349–355.21. Han SB, Bae EY, Lee JW, Lee DG, Chung NG, Jeong DC, et al. Clinical characteristics and antibiotic susceptibility of viridans streptococcal bacteremia in children with febrile neutropenia. Infection. 2013; 41:917–924.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Etiological Agents in Bacteremia of Children with Hemato-oncologic Diseases (2006-2010): A Single Center Study
- A Survey for Causative Organisms and Antimicrobial Susceptabilities of Bacteremia in a Single Center Children with Hemato-Oncologic Diseases (2004~2006)
- Clinical Investigation of Bacteremia in Children with Hemato-Oncologic Diseases
- Bloodstream Infections in Children with Cancer between 2005 and 2008 in a Single Center
- Underlying Hemato-oncologic, Gastrointestinal-nutritional Diseases, or Prematurity May Be Risk Factors for Hypovitaminosi D in Children