J Korean Med Sci.
2017 Oct;32(10):1642-1646. 10.3346/jkms.2017.32.10.1642.
Clinical Characteristics of Macrolide-Resistant Mycoplasma pneumoniae from Children in Jeju
- Affiliations
-
- 1Department of Pediatrics, Jeju National University Hospital, Jeju, Korea. ongsyunju@gmail.com
- 2Department of Pediatrics, Gyeongsang National University Changwon Hospital, Changwon, Korea.
- 3Department of Microbiology and Immunology, Jeju National University School of Medicine, Jeju, Korea.
- 4Department of Laboratory Medicine, Jeju National University Hospital, Jeju, Korea.
- KMID: 2400436
- DOI: http://doi.org/10.3346/jkms.2017.32.10.1642
Abstract
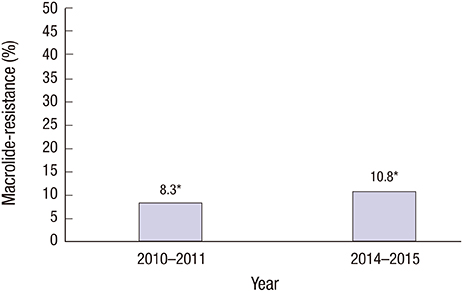
- Mycoplasma pneumoniae is the major pathogen of community-acquired pneumonia in children. The prevalence of macrolide-resistant M. pneumoniae (MRMP) is important owing to the limited alternative therapies for children. We analyzed 111 M. pneumoniae obtained from 107 children admitted for lower respiratory tract infection at Jeju National University Hospital between 2010 and 2015. Macrolide resistance of M. pneumoniae was searched for using polymerase chain reaction (PCR) and sequencing. Of 107 clinical M. pneumoniae, 11 (10.3%) carried macrolide resistance mutations in the 23S rRNA gene. All macrolide resistance mutations were A2063G transitions. We found an acquired A2063G mutation of M. pneumoniae from a patient during macrolide treatment. Patients' characteristics and clinical severity did not differ between those with MRMP and macrolide-sensitive M. pneumoniae, with the exception of frequent pleural effusion in the MRMP group. The prevalence of MRMP (10.3%) in Jeju Island was relatively lower than those of surrounding countries in East Asia. Previous antimicrobial usage and timing of diagnostic test should be considered when determining of macrolide resistance of M. pneumoniae.
Keyword
MeSH Terms
Figure
Reference
-
1. Waites KB, Talkington DF. Mycoplasma pneumoniae and its role as a human pathogen. Clin Microbiol Rev. 2004; 17:697–728.2. Foy HM, Kenny GE, Cooney MK, Allan ID. Long-term epidemiology of infections with Mycoplasma pneumoniae . J Infect Dis. 1979; 139:681–687.3. Hauksdottir GS, Love A, Sigurdardottir V, Jonsson T. Outbreaks of Mycoplasma pneumoniae infections in Iceland 1987 to 1997 - a ten and a half years review. Eur J Epidemiol. 1999; 15:95–96.4. Ito I, Ishida T, Osawa M, Arita M, Hashimoto T, Hongo T, Mishima M. Culturally verified Mycoplasma pneumoniae pneumonia in Japan: a long-term observation from 1979–99. Epidemiol Infect. 2001; 127:365–367.5. Eun BW, Kim NH, Choi EH, Lee HJ. Mycoplasma pneumoniae in Korean children: the epidemiology of pneumonia over an 18-year period. J Infect. 2008; 56:326–331.6. Morozumi M, Iwata S, Hasegawa K, Chiba N, Takayanagi R, Matsubara K, Nakayama E, Sunakawa K, Ubukata K; Acute Respiratory Diseases Study Group. Increased macrolide resistance of Mycoplasma pneumoniae in pediatric patients with community-acquired pneumonia. Antimicrob Agents Chemother. 2008; 52:348–350.7. Liu Y, Ye X, Zhang H, Xu X, Li W, Zhu D, Wang M. Antimicrobial susceptibility of Mycoplasma pneumoniae isolates and molecular analysis of macrolide-resistant strains from Shanghai, China. Antimicrob Agents Chemother. 2009; 53:2160–2162.8. Hong KB, Choi EH, Lee HJ, Lee SY, Cho EY, Choi JH, Kang HM, Lee J, Ahn YM, Kang YH, et al. Macrolide resistance of Mycoplasma pneumoniae, South Korea, 2000–2011. Emerg Infect Dis. 2013; 19:1281–1284.9. Zheng X, Lee S, Selvarangan R, Qin X, Tang YW, Stiles J, Hong T, Todd K, Ratliff AE, Crabb DM, et al. Macrolide-resistant Mycoplasma pneumoniae, United States. Emerg Infect Dis. 2015; 21:1470–1472.10. Oh CE, Choi EH, Lee HJ. Detection of genetic mutations associated with macrolide resistance of Mycoplasma pneumoniae . Korean J Pediatr. 2010; 53:178–183.11. Jain S, Williams DJ, Arnold SR, Ampofo K, Bramley AM, Reed C, Stockmann C, Anderson EJ, Grijalva CG, Self WH, et al. Community-acquired pneumonia requiring hospitalization among U.S. children. N Engl J Med. 2015; 372:835–845.12. Morozumi M, Takahashi T, Ubukata K. Macrolide-resistant Mycoplasma pneumoniae: characteristics of isolates and clinical aspects of community-acquired pneumonia. J Infect Chemother. 2010; 16:78–86.13. Okazaki N, Narita M, Yamada S, Izumikawa K, Umetsu M, Kenri T, Sasaki Y, Arakawa Y, Sasaki T. Characteristics of macrolide-resistant Mycoplasma pneumoniae strains isolated from patients and induced with erythromycin in vitro. Microbiol Immunol. 2001; 45:617–620.14. Zhao F, Liu G, Wu J, Cao B, Tao X, He L, Meng F, Zhu L, Lv M, Yin Y, et al. Surveillance of macrolide-resistant Mycoplasma pneumoniae in Beijing, China, from 2008 to 2012. Antimicrob Agents Chemother. 2013; 57:1521–1523.15. Eshaghi A, Memari N, Tang P, Olsha R, Farrell DJ, Low DE, Gubbay JB, Patel SN. Macrolide-resistant Mycoplasma pneumoniae in humans, Ontario, Canada, 2010–2011. Emerg Infect Dis. 2013; 19:1525–1527.16. Okada T, Morozumi M, Tajima T, Hasegawa M, Sakata H, Ohnari S, Chiba N, Iwata S, Ubukata K. Rapid effectiveness of minocycline or doxycycline against macrolide-resistant Mycoplasma pneumoniae infection in a 2011 outbreak among Japanese children. Clin Infect Dis. 2012; 55:1642–1649.17. Lee E, Cho HJ, Hong SJ, Lee J, Sung H, Yu J. Prevalence and clinical manifestations of macrolide resistant Mycoplasma pneumoniae pneumonia in Korean children. Korean J Pediatr. 2017; 60:151–157.18. Chironna M, Sallustio A, Esposito S, Perulli M, Chinellato I, Di Bari C, Quarto M, Cardinale F. Emergence of macrolide-resistant strains during an outbreak of Mycoplasma pneumoniae infections in children. J Antimicrob Chemother. 2011; 66:734–737.19. Averbuch D, Hidalgo-Grass C, Moses AE, Engelhard D, Nir-Paz R. Macrolide resistance in Mycoplasma pneumoniae, Israel, 2010. Emerg Infect Dis. 2011; 17:1079–1082.20. Wu PS, Chang LY, Lin HC, Chi H, Hsieh YC, Huang YC, Liu CC, Huang YC, Huang LM. Epidemiology and clinical manifestations of children with macrolide-resistant Mycoplasma pneumoniae pneumonia in Taiwan. Pediatr Pulmonol. 2013; 48:904–911.21. Cardinale F, Chironna M, Chinellato I, Principi N, Esposito S. Clinical relevance of Mycoplasma pneumoniae macrolide resistance in children. J Clin Microbiol. 2013; 51:723–724.22. Yoon IA, Hong KB, Lee HJ, Yun KW, Park JY, Choi YH, Kim WS, Lee H, Eun BW, Ahn YM, et al. Radiologic findings as a determinant and no effect of macrolide resistance on clinical course of Mycoplasma pneumoniae pneumonia. BMC Infect Dis. 2017; 17:402.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of the characteristics of macrolide-sensitive and macrolide-resistant Mycoplasma pneumoniae pneumonia requiring hospitalization in children
- Clinical issues regarding increased macrolide-resistant Mycoplasma pneumoniae in children
- Prevalence and clinical manifestations of macrolide resistant Mycoplasma pneumoniae pneumonia in Korean children
- Macrolide-refractory Mycoplasma pneumoniae pneumonia and hemophagocytic lymphohistiocytosis: case report and literature review
- Current perspectives on atypical pneumonia in children