J Clin Neurol.
2014 Jan;10(1):59-63.
Unilateral Reversible Posterior Leukoencephalopathy Syndrome after Coiling of an Aneurysm
- Affiliations
-
- 1Department of Neurology, MCH Westeinde Hospital, The Hague, The Netherlands. w.huijgen@mchaaglanden.nl
Abstract
- BACKGROUND
Reversible posterior leukoencephalopathy syndrome (RPLS) is radiologically characterized by symmetrical subcortical areas of vasogenic edema that are preferentially parieto-occipital, and it typically resolves after appropriate treatment.
CASE REPORT
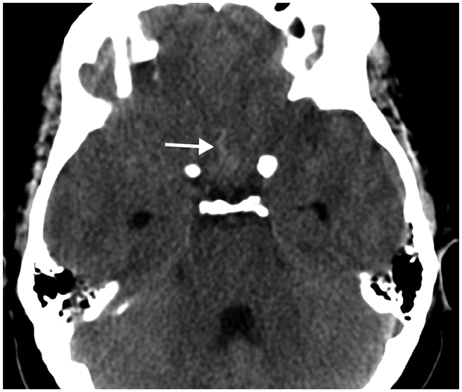
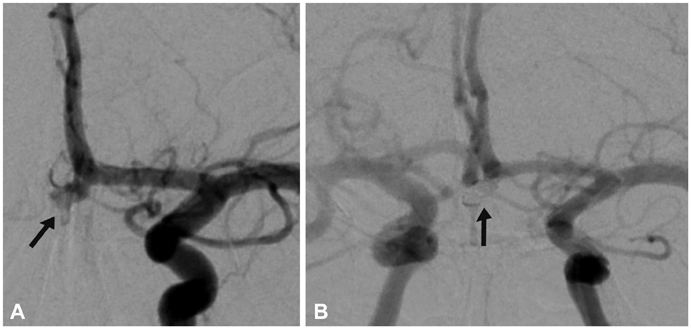
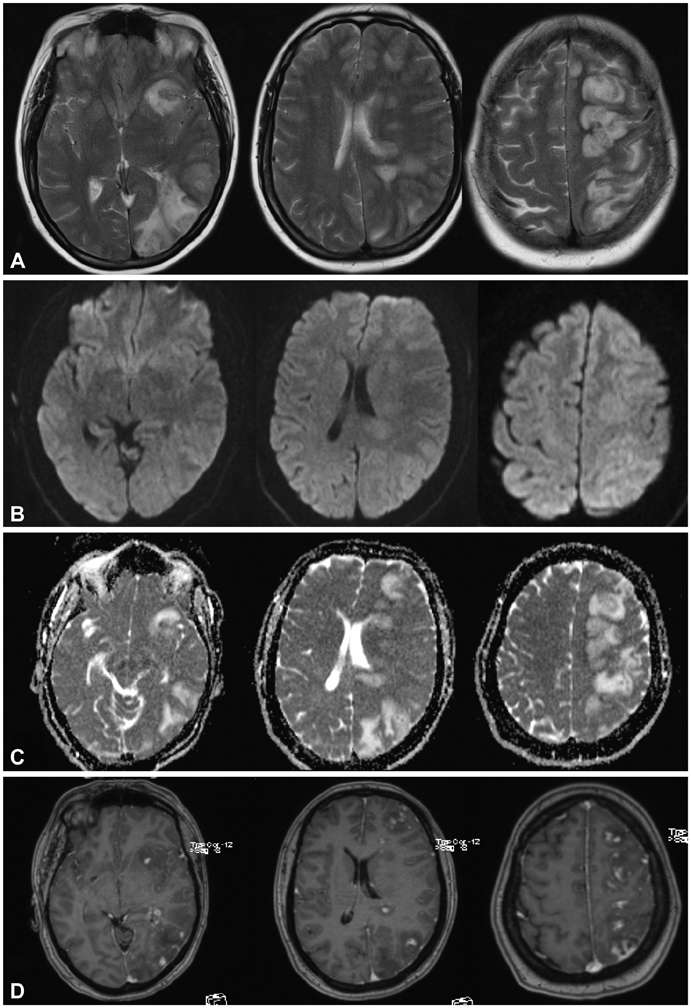
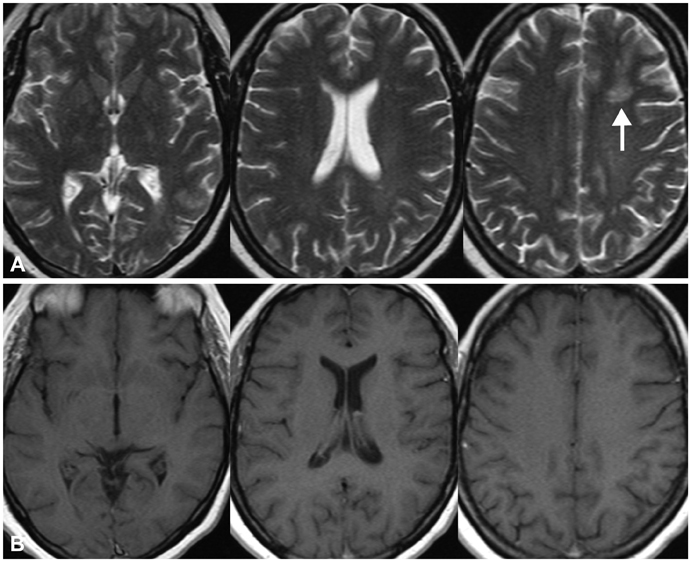
We present a patient with strikingly unilateral RPLS that developed 21 days after coiling of an anterior communicating artery aneurysm and several days of triple-H therapy. Cortical and subcortical vasogenic edema and enhancement developed only in the left hemisphere, with a pattern suggesting RPLS. After 7 months the lesions had nearly completely resolved.
CONCLUSIONS
The pathophysiological mechanism underlying RPLS is still not well understood, which makes it difficult to explain the unilateral appearance in this case. Since the imaging findings may be confused with other conditions such as ischemia, recognition of RPLS after coiling is necessary in order to avoid inadequate treatment.
Keyword
MeSH Terms
Figure
Reference
-
1. Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996; 334:494–500.
Article2. Bartynski WS. Posterior reversible encephalopathy syndrome, part 1: fundamental imaging and clinical features. AJNR Am J Neuroradiol. 2008; 29:1036–1042.
Article3. Stott VL, Hurrell MA, Anderson TJ. Reversible posterior leukoencephalopathy syndrome: a misnomer reviewed. Intern Med J. 2005; 35:83–90.
Article4. Fugate JE, Claassen DO, Cloft HJ, Kallmes DF, Kozak OS, Rabinstein AA. Posterior reversible encephalopathy syndrome: associated clinical and radiologic findings. Mayo Clin Proc. 2010; 85:427–432.
Article5. Bartynski WS, Boardman JF. Distinct imaging patterns and lesion distribution in posterior reversible encephalopathy syndrome. AJNR Am J Neuroradiol. 2007; 28:1320–1327.
Article6. Medel R, Crowley RW, Dumont AS. Hyperperfusion syndrome following endovascular cerebral revascularization. Neurosurg Focus. 2009; 26:E4.
Article7. Schaefer PW. Diffusion-weighted imaging as a problem-solving tool in the evaluation of patients with acute strokelike syndromes. Top Magn Reson Imaging. 2000; 11:300–309.
Article8. Schambra HM, Greer DM. Asymmetric reversible posterior leukoencephalopathy syndrome. Neurocrit Care. 2006; 4:245–247.
Article9. McKinney AM, Short J, Truwit CL, McKinney ZJ, Kozak OS, Santa-Cruz KS, et al. Posterior reversible encephalopathy syndrome: incidence of atypical regions of involvement and imaging findings. AJR Am J Roentgenol. 2007; 189:904–912.
Article10. Giraldo EA, Fugate JE, Rabinstein AA, Lanzino G, Wijdicks EF. Posterior reversible encephalopathy syndrome associated with hemodynamic augmentation in aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2011; 14:427–432.
Article11. Sanelli PC, Jacobs MA, Ougorets I, Mifsud MJ. Posterior reversible encephalopathy syndrome on computed tomography perfusion in a patient on "triple H" therapy. Neurocrit Care. 2005; 3:46–50.
Article12. Wartenberg KE, Parra A. CT and CT-perfusion findings of reversible leukoencephalopathy during triple-H therapy for symptomatic subarachnoid hemorrhage-related vasospasm. J Neuroimaging. 2006; 16:170–175.
Article13. Jang HW, Lee HJ. Posterior reversible leukoencephalopathy due to "triple H" therapy. J Clin Neurosci. 2010; 17:1059–1061.
Article14. Voetsch B, Tarlov N, Nguyen TN, DeFusco C, Barest GD, Norbash A, et al. Asymmetric posterior reversible encephalopathy syndrome complicating hemodynamic augmentation for subarachnoid hemorrhage-associated cerebral vasospasm. Neurocrit Care. 2011; 15:542–546.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- RE: Comments on "Unilateral Reversible Posterior Leukoencephalopathy Syndrome after Coiling of an Aneurysm": The Authors Respond
- Comments on "Unilateral Reversible Posterior Leukoencephalopathy Syndrome after Coiling of an Aneurysm"
- Reversible Posterior Leukoencephalopathy Syndrome(RPLS): with special reference to Brain MRA
- A Case of Posterior Reversible Leukoencephalopathy Syndrome Following Poststreptococcal Glomerulonephritis
- A Case of Reversible Posterior Leukoencephalopathy Syndrome associated with Low dose Intravenous Immunoglobulin Therapy after Induction Chemotherapy in Acute Myeloid Leukemia