J Periodontal Implant Sci.
2017 Dec;47(6):363-371. 10.5051/jpis.2017.47.6.363.
A randomized controlled clinical study of periodontal tissue regeneration using an extracellular matrix-based resorbable membrane in combination with a collagenated bovine bone graft in intrabony defects
- Affiliations
-
- 1Department of Periodontology, Seoul National University School of Dentistry, Seoul, Korea. kst72@snu.ac.kr
- 2ESTeam Paris Sud, INSERM UMR-S 935, Paris-Sud University, Paris-Saclay University, Villejuif, France.
- 3Department of Oral and Maxillofacial Surgery, Seoul National University School of Dentistry, Seoul, Korea. leejongh@snu.ac.kr
- KMID: 2399742
- DOI: http://doi.org/10.5051/jpis.2017.47.6.363
Abstract
- PURPOSE
The purpose of this study was to investigate the feasibility of regenerative therapy with a collagenated bone graft and resorbable membrane in intrabony defects, and to evaluate the effects of the novel extracellular matrix (ECM)-based membrane clinically and radiologically.
METHODS
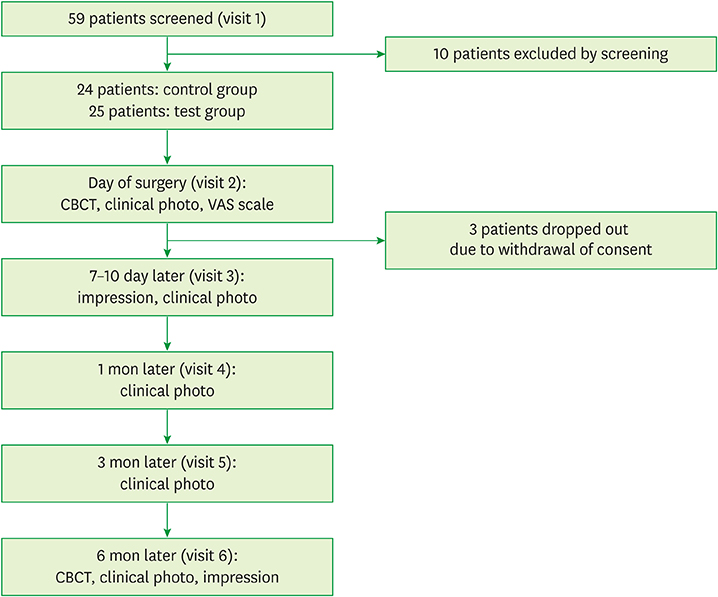
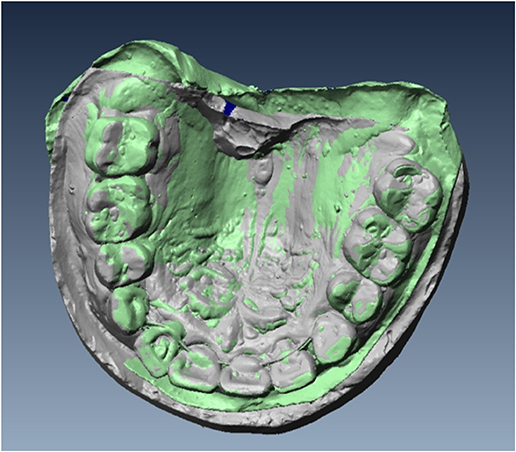
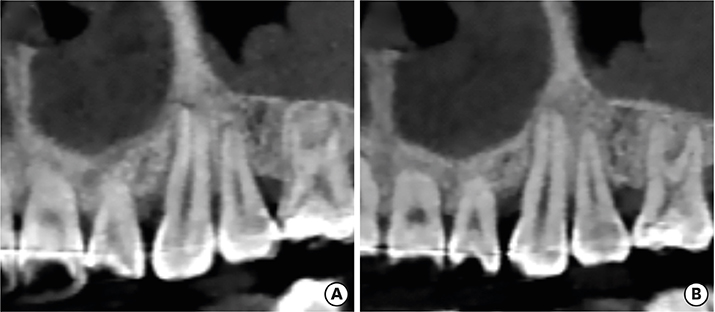
Periodontal tissue regeneration procedure was performed using an ECM-based resorbable membrane in combination with a collagenated bovine bone graft in intrabony defects around the teeth and implants. A novel extracellular matrix membrane (NEM) and a widely-used membrane (WEM) were randomly applied to the test group and the control group, respectively. Cone-beam computed tomography images were obtained on the day of surgery and 6 months after the procedure. Alginate impressions were taken and plaster models were made 1 week and 6 months postoperatively.
RESULTS
The quantity of bone tissue, the dimensional changes of the surgically treated intrabony defects, and the changes in width and height below the grafted bone substitutes showed no significant difference between the test and control groups at the 6-month examination.
CONCLUSIONS
The use of NEM for periodontal regeneration with a collagenated bovine bone graft showed similar clinical and radiologic results to those obtained using WEM.
Keyword
MeSH Terms
Figure
Reference
-
1. Paolantonio M. Combined periodontal regenerative technique in human intrabony defects by collagen membranes and anorganic bovine bone. A controlled clinical study. J Periodontol. 2002; 73:158–166.
Article2. Kiany F, Moloudi F. Amnion membrane as a novel barrier in the treatment of intrabony defects: a controlled clinical trial. Int J Oral Maxillofac Implants. 2015; 30:639–647.
Article3. Becker J, Al-Nawas B, Klein MO, Schliephake H, Terheyden H, Schwarz F. Use of a new cross-linked collagen membrane for the treatment of dehiscence-type defects at titanium implants: a prospective, randomized-controlled double-blinded clinical multicenter study. Clin Oral Implants Res. 2009; 20:742–749.
Article4. Ortolani E, Quadrini F, Bellisario D, Santo L, Polimeni A, Santarsiero A. Mechanical qualification of collagen membranes used in dentistry. Ann Ist Super Sanita. 2015; 51:229–235.5. Park JI, Yang C, Kim YT, Kim MS, Lee JS, Choi SH, et al. Space maintenance using crosslinked collagenated porcine bone grafted without a barrier membrane in one-wall intrabony defects. J Biomed Mater Res B Appl Biomater. 2014; 102:1454–1461.
Article6. Wikesjö UM, Lim WH, Thomson RC, Hardwick WR. Periodontal repair in dogs: gingival tissue occlusion, a critical requirement for GTR? J Clin Periodontol. 2003; 30:655–664.
Article7. Reynolds MA, Aichelmann-Reidy ME, Branch-Mays GL, Gunsolley JC. The efficacy of bone replacement grafts in the treatment of periodontal osseous defects. A systematic review. Ann Periodontol. 2003; 8:227–265.
Article8. Needleman I, Tucker R, Giedrys-Leeper E, Worthington H. A systematic review of guided tissue regeneration for periodontal infrabony defects. J Periodontal Res. 2002; 37:380–388.
Article9. Nevins ML, Camelo M, Lynch SE, Schenk RK, Nevins M. Evaluation of periodontal regeneration following grafting intrabony defects with bio-oss collagen: a human histologic report. Int J Periodontics Restorative Dent. 2003; 23:9–17.10. Nevins ML, Camelo M, Rebaudi A, Lynch SE, Nevins M. Three-dimensional micro-computed tomographic evaluation of periodontal regeneration: a human report of intrabony defects treated with Bio-Oss collagen. Int J Periodontics Restorative Dent. 2005; 25:365–373.11. Slotte C, Lindfors N, Nannmark U. Surgical reconstruction of peri-implant bone defects with prehydrated and collagenated porcine bone and collagen barriers: case presentations. Clin Implant Dent Relat Res. 2013; 15:714–723.
Article12. Sheikh Z, Hamdan N, Ikeda Y, Grynpas M, Ganss B, Glogauer M. Natural graft tissues and synthetic biomaterials for periodontal and alveolar bone reconstructive applications: a review. Biomater Res. 2017; 21:9.
Article13. Hwang JW, Kim S, Kim SW, Lee JH. Effect of extracellular matrix membrane on bone formation in a rabbit tibial defect model. BioMed Res Int. 2016; 2016:6715295.
Article14. Jiménez Garcia J, Berghezan S, Caramês JM, Dard MM, Marques DN. Effect of cross-linked vs non-cross-linked collagen membranes on bone: a systematic review. J Periodontal Res. 2017; 52:955–964.
Article15. Needleman IG, Worthington HV, Giedrys-Leeper E, Tucker RJ. Guided tissue regeneration for periodontal infra-bony defects. Cochrane Database Syst Rev. 2006; CD001724.
Article16. Grimard BA, Hoidal MJ, Mills MP, Mellonig JT, Nummikoski PV, Mealey BL. Comparison of clinical, periapical radiograph, and cone-beam volume tomography measurement techniques for assessing bone level changes following regenerative periodontal therapy. J Periodontol. 2009; 80:48–55.
Article17. Schwarz F, Sahm N, Mihatovic I, Golubovic V, Becker J. Surgical therapy of advanced ligature-induced peri-implantitis defects: cone-beam computed tomographic and histological analysis. J Clin Periodontol. 2011; 38:939–949.
Article18. Sculean A, Stavropoulos A, Windisch P, Keglevich T, Karring T, Gera I. Healing of human intrabony defects following regenerative periodontal therapy with a bovine-derived xenograft and guided tissue regeneration. Clin Oral Investig. 2004; 8:70–74.
Article19. Tonetti MS, Fourmousis I, Suvan J, Cortellini P, Bragger U, Lang NP, et al. Healing, post-operative morbidity and patient perception of outcomes following regenerative therapy of deep intrabony defects. J Clin Periodontol. 2004; 31:1092–1098.
Article20. Chang H, Kim S, Hwang JW, Kim S, Koo KT, Kim TI, et al. Comparative, randomized, double-blind clinical study of alveolar ridge preservation using an extracellular matrix-based dental resorbable membrane in the extraction socket. J Periodontal Implant Sci. 2017; 47:165–173.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Additional use of autogenous periosteal barrier membrane combined with regenerative therapy in the interproximal intrabony defects: case series
- The effects of Acellular dermal matrix on the healing of 1 wall intrabony defects in dogs
- Bone Regeneration Using Collagenated Synthetic Bone Graft Attached to Collagen Membrane with 3,4-dihydroxy-L-phenylalanine (DOPA)
- BBP(R) graft for periodontal intrabony defects and molar furcation lesions: Case Report
- Clinical effects of combination anorganic bovine-derived hydroxyapatite matrix(ABM)/cell binding peptide (P-15) in periodontal intrabony defects