Korean J Health Promot.
2017 Dec;17(4):242-251. 10.15384/kjhp.2017.17.4.242.
Inquiry Survey of Infertile Couples for Sperm Donation and Artificial Insemination by Donor
- Affiliations
-
- 1Department of Family Medicine, BHS Hanseo Hospital, Busan, Korea.
- 2The Korea Institution for Public Sperm Bank, Busan, Korea. pnc@pusan.ac.kr
- 3Department of Urology, Pusan National University School of Medicine, Busan, Korea.
- 4Department of Statistics, Pusan National University, Busan, Korea.
- KMID: 2399334
- DOI: http://doi.org/10.15384/kjhp.2017.17.4.242
Abstract
- BACKGROUND
Artificial insemination by donor (AID) is important to chance the pregnancy in male infertile couples by requiring appropriate medical, legal and ethical reviews. The purpose of this study was to investigate the perception changes of AID to collect the basic information for establishing the sperm donation, cryopreservation and artificial insemination management system.
METHODS
We evaluated the people's thought of sperm donation, cryopreservation, and artificial insemination by donor by means of national inquiry survey from 247 infertile couples for 4 weeks from October 2016. The questionnaires were composed of 4 areas, and each questionnaire consisted of 15 items. Changes in the perception of AID by year were investigated after review of domestic journals.
RESULTS
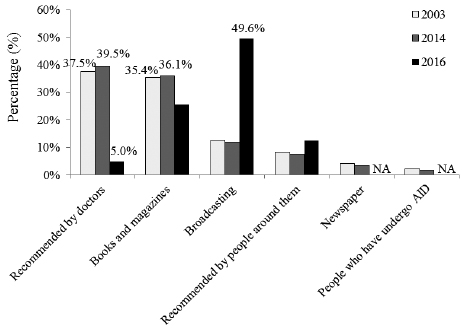
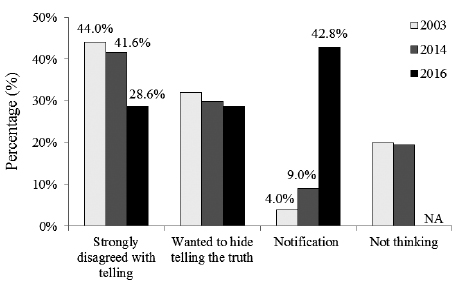
67.6% of respondents knew the growth of couples with difficulty getting pregnant due to male infertility. 82.2% of respondents replied the necessary of sperm bank as a treatment option for infertility and 40.5% knew the donation and receipt system of sperm. In the survey of change perception of AID according to year, 37.5% and 39.5% of respondents were got information about AID from doctor in 2003 and 2004, but 49.6% from broadcasting in 2016. As a child grows up, 4.0% (2003), 9.0% (2014), and 42.8% (2016) of respondents answered to tell the child about AID.
CONCLUSIONS
Infertile couple's thought of AID about the extension of opportunities for male infertility treatment is changed. In conclusion, it is necessary to establish institutional system of sperm donation, cryopreservation and artificial insemination prior to public sperm bank operation.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Comparative analysis of medical, legal, and ethical considerations for establishing a standard operating protocol for artificial insemination by donor
Min Jung Park
J Korean Med Assoc. 2018;61(7):383-391. doi: 10.5124/jkma.2018.61.7.383.Reasons of shortage for donated sperm and plan to resolve deficiencies in the sperm donor system
Nam Cheol Park
J Korean Med Assoc. 2018;61(7):408-415. doi: 10.5124/jkma.2018.61.7.408.
Reference
-
1. Nachtigall RD, Tschann JM, Quiroga SS, Pitcher L, Becker G. Stigma, disclosure, and family functioning among parents of children conceived through donor insemination. Fertil Steril. 1997; 68(1):83–89.
Article2. Vloeberghs V, Verheyen G, Haentjens P, Goossens A, Polyzos NP, Tournaye H. How successful is TESE-ICSI in couples with non-obstructive azoospermia? Hum Reprod. 2015; 30(8):1790–1796.
Article3. Hann SK, Kang HS. Infertile women's perception on the national support program for infertile couples. Korean J Women Health Nurs. 2015; 21(3):171–183.
Article4. Kantartzi PD, Goulis ChD, Goulis GD, Papadimas I. Male infertility and varicocele: myths and reality. Hippokratia. 2007; 11(3):99–104.5. Park NC. The current status of public sperm bank in Korea. J Korean Med Assoc. 2016; 59(3):194–204.
Article6. Sunderam S, Kissin DM, Crawford SB, Folger SG, Jamieson DJ, Warner L, et al. Assisted reproductive technology surveillance - United States, 2014. MMWR Surveill Summ. 2017; 66(6):1–24.
Article7. Linden JV, Centola G. New American association of tissue banks standards for semen banking. Fertil Steril. 1997; 68(4):597–600.
Article8. Gazvani R, Hamilton MP, Simpson SA, Templeton A. New challenges for gamete donation programmes: changes in guidelines are needed. Hum Fertil (Camb). 2002; 5(4):183–184.
Article9. Scandinavian recommendations: sperm donation. Bull Med Ethics. 2003; (191):8–9.10. Ethics Committee of the American Society for Reproductive Medicine. Interests, obligations, and rights in gamete donation: a committee opinion. Fertil Steril. 2014; 102(3):675–681.11. British Andrology Society. British Andrology Society guidelines for the screening of semen donors for donor insemination (1999). Hum Reprod. 1999; 14(7):1823–1826.12. Kim SC. The legal standing of children born under AID. Law review. 2011; 41:85–108.13. Park HJ, Park NC. An attitude survey of male infertile patients with artificial insemination by donor. Korean J Fertil Steril. 2003; 30(4):281–291.14. Hwang DS, Jeon TG, Park HJ, Park NC. The attitudes of infertile male patients toward the use of artificial insemination by donor: a Korean regional survey. Korean J Urol. 2014; 55(2):134–139.
Article15. Moon H, Park SY, Kim MH. Online monitoring about illegal Surrogacy arrangement on a commercial basis in Korea. Korean J Med Ethics. 2016; 19(1):36–46.16. Shiai C. Reproductive technologies and parent–child relationships: Japan's past and present examined through the lens of donor insemination. Int J Jpn Sociol. 2010; 19(1):18–34.17. Liao J, Dessein B, Pennings G. The ethical debate on donor insemination in China. Reprod Biomed Online. 2010; 20(7):895–902.
Article18. Pi VL. Regulating sperm donation: why requiring exposed donation is not the answer. Duke J Gend Law Policy. 2009; 16:379–401.19. Sabatello M. Regulating gamete donation in the U.S.: ethical, legal and social implications. Laws. 2015; 4(3):352–376.
Article20. Gong D, Liu YL, Zheng Z, Tian YF, Li Z. An overview on ethical issues about sperm donation. Asian J Androl. 2009; 11(6):645–652.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Attitudes of Infertile Male Patients Toward the Use of Artificial Insemination by Donor: A Korean Regional Survey
- Reasons of shortage for donated sperm and plan to resolve deficiencies in the sperm donor system
- Comparative analysis of medical, legal, and ethical considerations for establishing a standard operating protocol for artificial insemination by donor
- The current status of public sperm bank in Korea
- An attitude survey of male infertile patients with artificial insemination by donor