Ann Surg Treat Res.
2017 Sep;93(3):166-169. 10.4174/astr.2017.93.3.166.
Pectoral nerve block (Pecs block) with sedation for breast conserving surgery without general anesthesia
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, College of Medicine, Kyung Hee University, Seoul, Korea. mdyjwchk@khu.ac.kr
- 2Department of Surgery, College of Medicine, Kyung Hee University, Seoul, Korea.
- KMID: 2398964
- DOI: http://doi.org/10.4174/astr.2017.93.3.166
Abstract
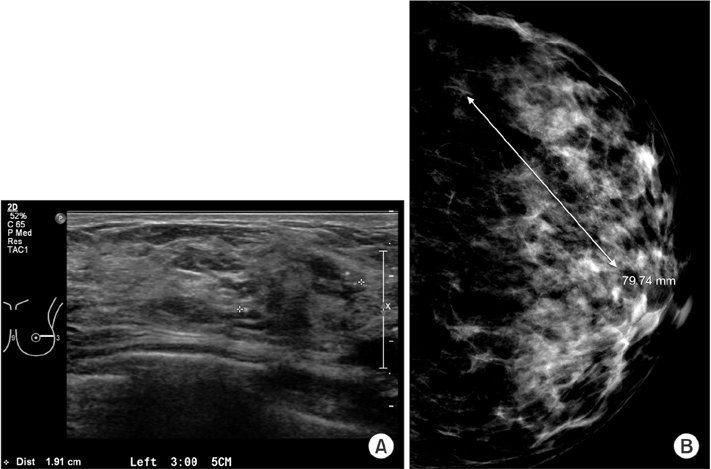
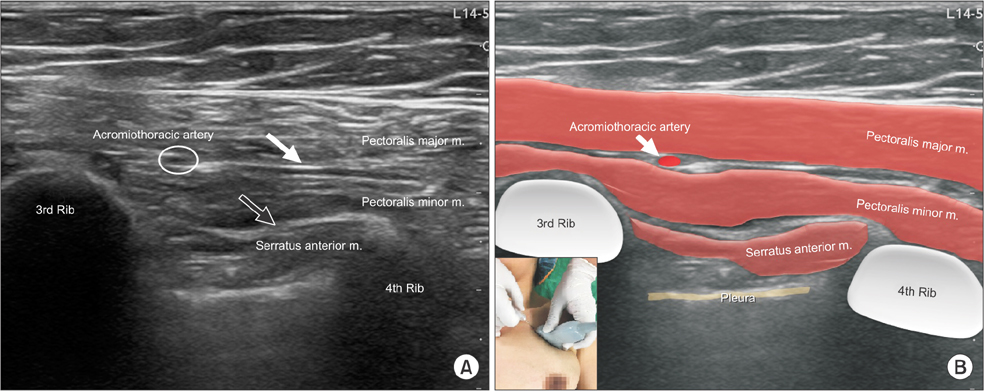
- Most regional anesthesia in breast surgeries is performed as postoperative pain management under general anesthesia, and not as the primary anesthesia. Regional anesthesia has very few cardiovascular or pulmonary side-effects, as compared with general anesthesia. Pectoral nerve block is a relatively new technique, with fewer complications than other regional anesthesia. We performed Pecs I and Pec II block simultaneously as primary anesthesia under moderate sedation with dexmedetomidine for breast conserving surgery in a 49-year-old female patient with invasive ductal carcinoma. Block was uneventful and showed no complications. Thus, Pecs block with sedation could be an alternative to general anesthesia for breast surgeries.
MeSH Terms
Figure
Reference
-
1. Gartner R, Jensen MB, Nielsen J, Ewertz M, Kroman N, Kehlet H. Prevalence of and factors associated with persistent pain following breast cancer surgery. JAMA. 2009; 302:1985–1992.2. Batra RK, Krishnan K, Agarwal A. Paravertebral block. J Anaesthesiol Clin Pharmacol. 2011; 27:5–11.3. Blanco R, Fajardo M, Parras Maldonado T. Ultrasound description of Pecs II (modified Pecs I): a novel approach to breast surgery. Rev Esp Anestesiol Reanim. 2012; 59:470–475.4. Kairaluoma PM, Bachmann MS, Rosenberg PH, Pere PJ. Preincisional paravertebral block reduces the prevalence of chronic pain after breast surgery. Anesth Analg. 2006; 103:703–708.5. Bashandy GM, Abbas DN. Pectoral nerves I and II blocks in multimodal analgesia for breast cancer surgery: a randomized clinical trial. Reg Anesth Pain Med. 2015; 40:68–74.6. Voigt M, Frohlich CW, Waschke KF, Lenz C, Gobel U, Kerger H. Prophylaxis of postoperative nausea and vomiting in elective breast surgery. J Clin Anesth. 2011; 23:461–468.7. Manahan MA, Basdag B, Kalmar CL, Shridharani SM, Magarakis M, Jacobs LK, et al. Risk of severe and refractory postoperative nausea and vomiting in patients undergoing diep flap breast reconstruction. Microsurgery. 2014; 34:112–121.8. Fujiwara A, Komasawa N, Minami T. Pectoral nerves (PECS) and intercostal nerve block for cardiac resynchronization therapy device implantation. Springerplus. 2014; 3:409.9. Abdallah FW, Dwyer T, Chan VW, Niazi AU, Ogilvie-Harris DJ, Oldfield S, et al. IV and perineural dexmedetomidine similarly prolong the duration of analgesia after interscalene brachial plexus block: a randomized, three-arm, triple-masked, placebo-controlled trial. Anesthesiology. 2016; 124:683–695.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Thoracic interfascial nerve block for breast surgery in a pregnant woman: a case report
- PECS II block is associated with lower incidence of chronic pain after breast surgery
- Modified pectoral nerve block versus bi-level erector spinae plane block for postoperative analgesia after radical mastectomy surgery: a prospective, randomized, controlled trial
- Pectoral nerve blocks for transvenous subpectoral pacemaker insertion in children: a randomized controlled study
- Surgical excision of the breast giant fibroadenoma under regional anesthesia by Pecs II and internal intercostal plane block: a case report and brief technical description: a case report