J Rhinol.
2017 Nov;24(2):74-80. 10.18787/jr.2017.24.2.74.
Postoperative Septal Abscesses According to the Techniques of the Septoplasty
- Affiliations
-
- 1Department of Radiology, Eulji University Medical Center, College of Medicine, Eulji University, Daejeon, Korea.
- 2Department of Otolaryngology-Head and Neck Surgery, Eulji University Medical Center, College of Medicine, Eulji University, Daejeon, Korea. mschoi@eulji.ac.kr
- KMID: 2398824
- DOI: http://doi.org/10.18787/jr.2017.24.2.74
Abstract
- BACKGROUND AND OBJECTIVES
Recently, the swinging door and grafting techniques have been heavily used for straightening and holding the caudal septum. However, reconstructive septoplasties require more extensive dissection of septal structures. Extensive anatomical dissection and complicated procedures may affect the probability of postoperative bleeding and infection. MATERIALS AND METHOD: We retrospectively reviewed the records of 141 consecutive patients who underwent septal surgeries from February 2013 to December 2015. The patients were classified into two groups according to surgical technique: those who underwent submucous resection with or without endoscopy were classified as the "resection" group, while those who underwent the swinging door or batten graft technique were classified as the "reconstruction" group. The resection and reconstruction groups were matched using the propensity score. The incidence of postoperative septal abscesses (PSAs) was analyzed between the two groups.
RESULTS
For the two groups, 36 patients were matched with 36 patients (1:1) using the propensity score. Of the 72 patients, PSAs developed in 5 patients (6.9%). One patient was in the resection group (2.8%), while the other four patients were in the reconstruction group (11.1%). However, the incidence of PSAs was not significantly higher in the reconstruction group according to Fisher's exact test (p=0.164).
CONCLUSION
Reconstructive septoplasty resulted in more septal abscesses than resection, but the difference was not significant.
MeSH Terms
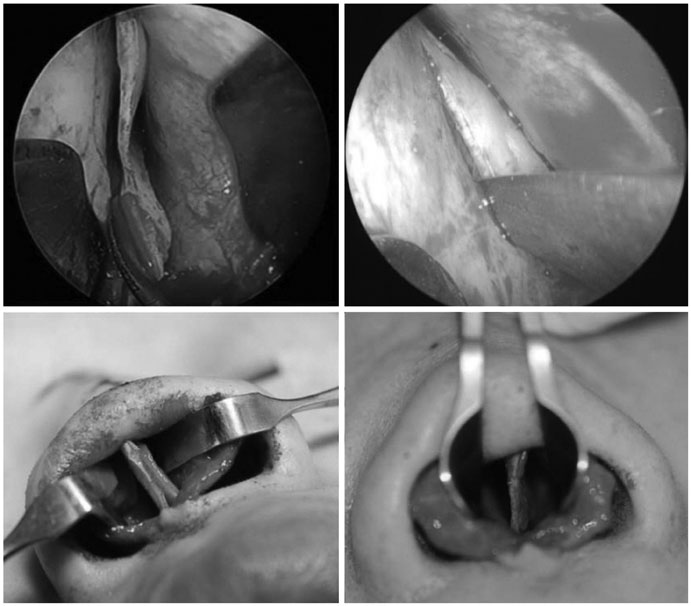
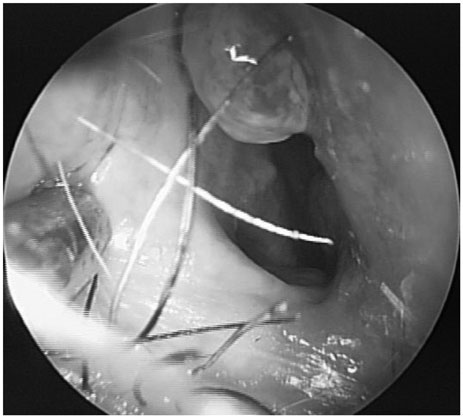
Figure
Reference
-
1. Sautter NB, Smith TL. Endoscopic septoplasty. Otolaryngol Clin North Am. 2009; 42(2):253–260.
Article2. Jin HR, Won TB. Septoplasty; Current concept and technique. J Rhinol. 2008; 15(1):13–29.3. Kim YD. Septoplasty and turbinoplasty; Current concept and technique. J Rhinol. 2012; 19(1):19–28.4. Rettinger G, Kirsche H. Complications in septoplasty. Facial Plast Surg. 2006; 22(4):289–297.
Article5. Schwab JA, Pirsig W. Complications of septal surgery. Facial Plast Surg. 1997; 13(1):3–14.
Article6. Yoder MG, Weimert TA. Antibiotics and topical surgical preparation solution in septal surgery. Otolaryngol Head Neck Surg. 1992; 106(3):243–244.
Article7. Mäkitie A, Aaltonen LM, Hytönen M, Malmberg H. Postoperative infection following nasal septoplasty. Acta Otolaryngol Suppl. 2000; 543:165–166.
Article8. Lee SB, Jang YJ. Treatment outcomes of extracorporeal septoplasty compared with in situ septal correction in rhinoplasty. JAMA Facial Plast Surg. 2014; 16(5):328–334.
Article9. Gubisch W. Extracorporeal septoplasty for the markedly deviated septum. Arch Facial Plast Surg. 2005; 7(4):218–226.
Article10. Pribitkin EA, Ezzat WH. Classification and treatment of the saddle nose deformity. Otolaryngol Clin North Am. 2009; 42(3):437–461.
Article11. Abuzeid WM, Brandt MG, Moyer JS, Baker SR. Methicillin-resistant Staphylococcus aureus-associated infections following septorhinoplasty. Facial Plast Surg. 2012; 28(3):354–357.
Article12. Kluytmans J, van Belkum A, Verbrugh H. Nasal carriage of Staphylococcus aureus: epidemiology, underlying mechanisms, and associated risks. Clin Microbiol Rev. 1997; 10(3):505–520.
Article13. Yoo DB, Peng GL, Azizzadeh B, Nassif PS. Microbiology and antibiotics prophylaxis in rhinoplasty: a review of 363 consecutive cases. JAMA Facial Plast Surg. 2015; 17(1):23–27.
Article14. Kaygusuz I, Kizirgil A, Karlidağ T, Yalçin S, Keles E, Yakupogullari Y, et al. Bacteriemia in septoplasty and septorhinoplasty surgery. Rhinology. 2003; 41(2):76–79.15. Okur E, Yildirim I, Aral M, et al. Bacteremia during open septorhinoplasty. Am J Rhinol. 2006; 20(1):36–39.
Article16. Andrews PJ, East CA, Jayaraj SM, Badia L, Panagamuwa C, Harding L. Prophylactic vs postoperative antibiotic use in complex septorhinoplasty surgery: a prospective, randomized, single-blind trial comparing efficacy. Arch Facial Plast Surg. 2006; 8(2):84–87.
Article17. Huber K, Bates ER, Valgimigli M, Wallentin L, Kristensen SD, Anderson JL, et al. Antiplatelet and anticoagulation agents in acute coronary syndromes: what is the current status and what does the future hold? Am heart J. 2014; 168(5):611–621.
Article