J Gastric Cancer.
2017 Dec;17(4):374-383. 10.5230/jgc.2017.17.e42.
Clinical Outcomes of Endoscopic Hemostasis for Bleeding in Patients with Unresectable Advanced Gastric Cancer
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine and Liver Research Institute, Seoul National University College of Medicine, Seoul, Korea. hschungmd@gmail.com
- 2Department of Internal Medicine, Institute of Gastroenterology, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 3Departtment of Medicine, Yonsei University Graduate School, Seoul, Korea.
- KMID: 2398803
- DOI: http://doi.org/10.5230/jgc.2017.17.e42
Abstract
- PURPOSE
Bleeding is one of the most serious complications of advanced gastric cancer (AGC) and is associated with a poor prognosis. This study aimed to evaluate the clinical outcomes of endoscopic hemostasis for bleeding in patients with unresectable AGC.
MATERIALS AND METHODS
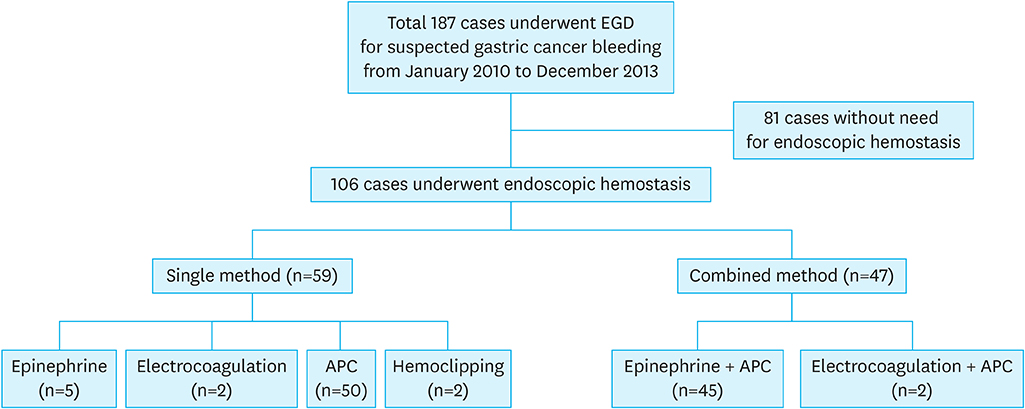
This study included 106 patients with bleeding associated with gastric cancer who had undergone endoscopic hemostasis between January 2010 and December 2013. Clinical characteristics, treatment outcomes, including rates of successful endoscopic hemostasis and rebleeding, risk factors for rebleeding, and overall survival (OS) were investigated.
RESULTS
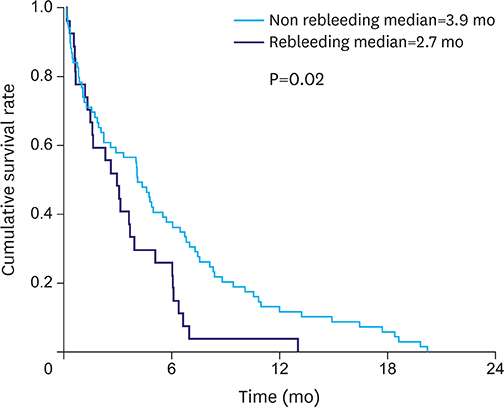
Successful initial hemostasis was achieved in 83% of patients. Rebleeding occurred in 28.3% of patients within 30 days. The median OS after initial hemostasis was lower in patients with rebleeding than in those without rebleeding (2.7 and 3.9 months, respectively, P=0.02). There were no significant differences in disease status and rebleeding rates among patients with partial response or stable disease (n=4), progressive disease (n=64), and first diagnosis of disease (n=38). Univariate and multivariate analyses (P=0.038 and 0.034, respectively) revealed that transfusion of ≥5 units of RBCs was a significant risk factor for rebleeding.
CONCLUSIONS
Despite favorable success rates of endoscopic hemostasis for bleeding associated with gastric cancer, the 30-day rebleeding rate was 28.3% and the median OS was significantly lower in patients with rebleeding than in those without rebleeding. Massive transfusion (≥5 units of RBCs) was the only significant risk factor for rebleeding. Patients with bleeding associated with AGC who have undergone massive transfusion should be observed closely following endoscopic hemostasis. Further research on approaches to reduce rebleeding rate and prevent death is needed.
Keyword
MeSH Terms
Figure
Reference
-
1. Muguruma N, Kitamura S, Kimura T, Miyamoto H, Takayama T. Endoscopic management of nonvariceal upper gastrointestinal bleeding: state of the art. Clin Endosc. 2015; 48:96–101.2. Klein A, Gralnek IM. Acute, nonvariceal upper gastrointestinal bleeding. Curr Opin Crit Care. 2015; 21:154–162.3. Laine L. Upper gastrointestinal tract hemorrhage. West J Med. 1991; 155:274–279.4. Loftus EV Jr, Alexander GL, Ahlquist DA, Balm RK. Endoscopic treatment of major bleeding from advanced gastroduodenal malignant lesions. Mayo Clin Proc. 1994; 69:736–740.5. Savides TJ, Jensen DM, Cohen J, Randall GM, Kovacs TO, Pelayo E, et al. Severe upper gastrointestinal tumor bleeding: endoscopic findings, treatment, and outcome. Endoscopy. 1996; 28:244–248.6. Sheibani S, Kim JJ, Chen B, Park S, Saberi B, Keyashian K, et al. Natural history of acute upper GI bleeding due to tumours: short-term success and long-term recurrence with or without endoscopic therapy. Aliment Pharmacol Ther. 2013; 38:144–150.7. Kim YI, Choi IJ, Cho SJ, Lee JY, Kim CG, Kim MJ, et al. Outcome of endoscopic therapy for cancer bleeding in patients with unresectable gastric cancer. J Gastroenterol Hepatol. 2013; 28:1489–1495.8. Laine L, Spiegel B, Rostom A, Moayyedi P, Kuipers EJ, Bardou M, et al. Methodology for randomized trials of patients with nonvariceal upper gastrointestinal bleeding: recommendations from an international consensus conference. Am J Gastroenterol. 2010; 105:540–550.9. Hwang JH, Fisher DA, Ben-Menachem T, Chandrasekhara V, Chathadi K, Decker GA, et al. The role of endoscopy in the management of acute non-variceal upper GI bleeding. Gastrointest Endosc. 2012; 75:1132–1138.10. Albeldawi M, Qadeer MA, Vargo JJ. Managing acute upper GI bleeding, preventing recurrences. Cleve Clin J Med. 2010; 77:131–142.11. Mathus-Vliegen EM, Tytgat GN. Analysis of failures and complications of neodymium: YAG laser photocoagulation in gastrointestinal tract tumors. A retrospective survey of 18 years' experience. Endoscopy. 1990; 22:17–23.12. Suzuki H, Miho O, Watanabe Y, Kohyama M, Nagao F. Endoscopic laser therapy in the curative and palliative treatment of upper gastrointestinal cancer. World J Surg. 1989; 13:158–164.13. Kwon JY, Yun J, Kim HJ, Kim KH, Kim SH, Lee SC, et al. Clinical outcome of gastric cancer patients with bone marrow metastases. Cancer Res Treat. 2011; 43:244–249.14. Heller SJ, Tokar JL, Nguyen MT, Haluszka O, Weinberg DS. Management of bleeding GI tumors. Gastrointest Endosc. 2010; 72:817–824.15. Akhtar K, Byrne JP, Bancewicz J, Attwood SE. Argon beam plasma coagulation in the management of cancers of the esophagus and stomach. Surg Endosc. 2000; 14:1127–1130.16. Zenker M. Argon plasma coagulation. GMS Krankenhhyg Interdiszip. 2008; 3:Doc15.17. Kwan V, Bourke MJ, Williams SJ, Gillespie PE, Murray MA, Kaffes AJ, et al. Argon plasma coagulation in the management of symptomatic gastrointestinal vascular lesions: experience in 100 consecutive patients with long-term follow-up. Am J Gastroenterol. 2006; 101:58–63.18. Vergara M, Bennett C, Calvet X, Gisbert JP. Epinephrine injection versus epinephrine injection and a second endoscopic method in high-risk bleeding ulcers. Cochrane Database Syst Rev. 2014; CD005584.19. Kasakura Y, Ajani JA, Mochizuki F, Morishita Y, Fujii M, Takayama T. Outcomes after emergency surgery for gastric perforation or severe bleeding in patients with gastric cancer. J Surg Oncol. 2002; 80:181–185.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Management of Tumor Bleeding from Inoperable Gastric Cancer
- Endoscopic Therapy for Acute Diverticular Bleeding
- Endoscopic Hemostasis for Bleeding Gastric Ulcer Caused by Ibuprofen in a 16-month-old Infant
- Clinical Evaluation of Endoscopic Microwave Coagulation Therapy for Upper Gastrointestinal Bleeding
- Endovascular hemostasis for endoscopic procedure-related gastrointestinal bleeding