J Korean Assoc Pediatr Surg.
2017 Dec;23(2):48-51. 10.13029/jkaps.2017.23.2.48.
Laparoscopic versus Open Herniorrhapy in Corrected Age 3 Months
- Affiliations
-
- 1Department of Pediatric Surgery, Asan Medical Center Children's Hospital, University of Ulsan College of Medicine, Seoul, Korea. kimdy@amc.seoul.kr
- KMID: 2398576
- DOI: http://doi.org/10.13029/jkaps.2017.23.2.48
Abstract
- PURPOSE
Inguinal hernia in early infant is a challenging surgical condition. This study aims to evaluate the efficacy and safety of laparoscopic inguinal hernia repair (LH) for small babies in corrected age 3 months compared with the traditional open inguinal hernia repair (OH).
METHODS
Medical records were retrospectively reviewed in 232 pediatric patients under corrected age 3 months who underwent inguinal hernia repair from January 1, 2013 to December 31, 2015. The chi-squared and Fisher's exact test were used to analyze the results of the study.
RESULTS
As for operative time, in unilateral/bilateral inguinal hernia repair, OH is faster than LH (p < 0.05 vs. p=0.06). But operation time gap is shorter in bilateral hernia than unilateral hernia. As for operation site, bilateral inguinal hernia case was more performed in LH than OH (p < 0.05). For comparison with the spontaneous breathing recovery time, there was no statistical difference between the two techniques (p=0.96). As for the recurrence rate, no significant difference was observed between the two techniques (p=0.36), whereas the relative risk of recurrence was higher for OH compared with LH (OR=1.56).
CONCLUSION
LH is also feasible and safe procedure as OH for small babies in corrected age 3 months for experienced pediatric surgeons.
Keyword
MeSH Terms
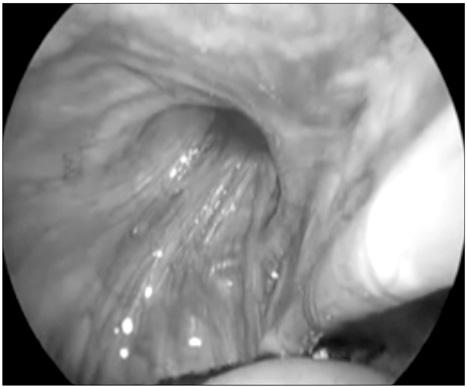
Figure
Reference
-
1. Pastore V, Bartoli F. Neonatal laparoscopic inguinal hernia repair: a 3-year experience. Hernia. 2015; 19:611–615.2. Shalaby R, Ibrahem R, Shahin M, Yehya A, Abdalrazek M, Alsayaad I, et al. Laparoscopic hernia repair versus open herniotomy in children: a controlled randomized study. Minim Invasive Surg. 2012; 2012:484135.3. Shalaby R, Ismail M, Dorgham A, Hefny K, Alsaied G, Gabr K, et al. Laparoscopic hernia repair in infancy and childhood: evaluation of 2 different techniques. J Pediatr Surg. 2010; 45:2210–2216.4. Schier F. Laparoscopic inguinal hernia repair-a prospective personal series of 542 children. J Pediatr Surg. 2006; 41:1081–1084.5. Cam C, Celik C, Sancak A, Iskender C, Karateke A. Inguinal herniorrhaphy in childhood may result in tubal damage and future infertility. Arch Gynecol Obstet. 2009; 279:175–176.6. Eshtewi SA. Laparoscopy complications in neonates and small infants. World J Laparosc Surg. 2008; 1:15–19.7. Hillier SC, Krishna G, Brasoveanu E. Neonatal anesthesia. Semin Pediatr Surg. 2004; 13:142–151.8. Turial S, Enders J, Krause K, Schier F. Laparoscopic inguinal herniorrhaphy in babies weighing 5 kg or less. Surg Endosc. 2011; 25:72–78.9. Chan IH, Lau CT, Chung PH, Chan KL, Lan LC, Wong KK, et al. Laparoscopic inguinal hernia repair in premature neonates: is it safe? Pediatr Surg Int. 2013; 29:327–330.10. Lee SL, Gleason JM, Sydorak RM. A critical review of premature infants with inguinal hernias: optimal timing of repair, incarceration risk, and postoperative apnea. J Pediatr Surg. 2011; 46:217–220.11. Lautz TB, Raval MV, Reynolds M. Does timing matter? A national perspective on the risk of incarceration in premature neonates with inguinal hernia. J Pediatr. 2011; 158:573–577.12. Schier F. Laparoscopic herniorrhaphy in girls. J Pediatr Surg. 1998; 33:1495–1497.13. Chan KL, Tam PK. Technical refinements in laparoscopic repair of childhood inguinal hernias. Surg Endosc. 2004; 18:957–960.14. Lee Y, Liang J. Experience with 450 cases of micro-laparoscopic herniotomy in infants and children. Pediatr Endo Surg Innov Tech. 2002; 6:25–28.15. Ron O, Eaton S, Pierro A. Systematic review of the risk of developing a metachronous contralateral inguinal hernia in children. Br J Surg. 2007; 94:804–811.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Extraperitoneal Laparoscopic Versus Open Burch Colposuspension for Treatment of Stress Urinary Incontinence: Long Term Follow-up
- Laparoscopic Cholecystectomy in Elderly Patients
- Open Versus Laparoscopic Splenectomy for Immune Thrombocytopenic Purpura
- A Comparative Study between Laparoscopic and Open Appendectomy in Childhood
- Comparison between Extraperitoneal Laparoscopic Burch Colposuspension Using Mesh and Tacker and Open Burch Procedure