J Breast Cancer.
2017 Dec;20(4):404-407. 10.4048/jbc.2017.20.4.404.
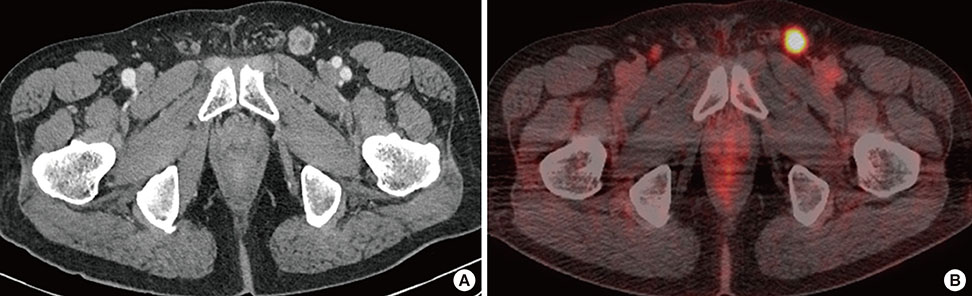
Ectopic Male Breast Cancer in the Perineum: A Case Report
- Affiliations
-
- 1Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 2Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. spdoctorko@gmail.com
- 3Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2398212
- DOI: http://doi.org/10.4048/jbc.2017.20.4.404
Abstract
- Ectopic breast tissue and male breast cancer are both very rare diseases with only a few reports in the literature. Here, we present the first case of ectopic male breast cancer in the perineum. The patient was a 70-year-old man with a palpable mass in the perineum. A wide local excision and inguinal lymph node dissection revealed invasive breast carcinoma of no special type involving the skin and subcutis, and inguinal lymph node metastases. Immunohistochemical staining showed that the tumor cells were strongly positive for estrogen and progesterone receptors and negative for human epidermal growth factor receptor 2. Moreover, no p53 overexpression was observed. Herein, the clinical and pathologic features, as well as a review of ectopic male breast cancer are discussed.
MeSH Terms
Figure
Reference
-
1. Nihon-Yanagi Y, Ueda T, Kameda N, Okazumi S. A case of ectopic breast cancer with a literature review. Surg Oncol. 2011; 20:35–42.
Article2. Hong JH, Oh MJ, Hur JY, Lee JK. Accessory breast tissue presenting as a vulvar mass in an adolescent girl. Arch Gynecol Obstet. 2009; 280:317–320.
Article3. Giordano SH, Cohen DS, Buzdar AU, Perkins G, Hortobagyi GN. Breast carcinoma in men: a population-based study. Cancer. 2004; 101:51–57.4. Gutermuth J, Audring H, Voit C, Haas N. Primary carcinoma of ectopic axillary breast tissue. J Eur Acad Dermatol Venereol. 2006; 20:217–221.
Article5. Wysokinska EM, Keeney G. Breast cancer occurring in the chest wall: rare presentation of ectopic milk line breast cancer. J Clin Oncol. 2014; 32:e35–e36.
Article6. Francone E, Nathan MJ, Murelli F, Bruno MS, Traverso E, Friedman D. Ectopic breast cancer: case report and review of the literature. Aesthetic Plast Surg. 2013; 37:746–749.
Article7. Marshall MB, Moynihan JJ, Frost A, Evans SR. Ectopic breast cancer: case report and literature review. Surg Oncol. 1994; 3:295–304.
Article8. Ghosn SH, Khatri KA, Bhawan J. Bilateral aberrant axillary breast tissue mimicking lipomas: report of a case and review of the literature. J Cutan Pathol. 2007; 34:Suppl 1. 9–13.
Article9. Cogswell HD, Czerny EW. Carcinoma of aberrant breast of the axilla. Am Surg. 1961; 27:388–390.10. Pardo M, Silva F, Jiménez P, Karmelic M. Mammary carcinoma in ectopic breast tissue: a case report. Rev Med Chil. 2001; 129:663–665.11. Greene HJ. Adenocarcinoma of supernumerary breasts of the labia majora in a case of epidermoid carcinoma of the vulva. Am J Obstet Gynecol. 1936; 31:660–663.
Article12. Gnerlich JL, Deshpande AD, Jeffe DB, Seelam S, Kimbuende E, Margenthaler JA. Poorer survival outcomes for male breast cancer compared with female breast cancer may be attributable to in-stage migration. Ann Surg Oncol. 2011; 18:1837–1844.
Article13. Yamamura J, Masuda N, Kodama Y, Yasojima H, Mizutani M, Kuriyama K, et al. Male breast cancer originating in an accessory mammary gland in the axilla: a case report. Case Rep Med. 2012; 2012:286210.
Article14. Markopoulos C, Kouskos E, Kontzoglou K, Gogas G, Kyriakou V, Gogas J. Breast cancer in ectopic breast tissue. Eur J Gynaecol Oncol. 2001; 22:157–159.15. Cripe J, Eskander R, Tewari K. Sentinel lymph node mapping of a breast cancer of the vulva: case report and literature review. World J Clin Oncol. 2015; 6:16–21.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Aberrant breast tissue of the perineum: a report on two cases
- Giant Axillary Ectopic Breast in a Male Patient: A Case Report
- Ductal Carcinoma Arising from Ectopic Breast Tissue Following Microcalcification Observed on Screening Mammography: A Case Report and Review of the Literature
- Ectopic Male Breast Cancer in Suprapubic Area That Relapsed with Hematogenous Metastasis
- The Therapeutic Effect of Cyclin-Dependent Kinase 4/6 Inhibitor on Relapsed Ectopic Male Breast Cancer