J Korean Ophthalmol Soc.
2017 Dec;58(12):1416-1419. 10.3341/jkos.2017.58.12.1416.
Multiple Subretinal and Intraretinal Hemorrhages as a First Sign of Infective Endocarditis
- Affiliations
-
- 1Department of Ophthalmology, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 2T2B Infrastructure Center for Ocular Disease, Inje University Busan Paik Hospital, Busan, Korea.
- 3Department of Ophthalmology, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea. maekbak@hanmail.net
- KMID: 2397857
- DOI: http://doi.org/10.3341/jkos.2017.58.12.1416
Abstract
- PURPOSE
To report a patient with multiple subretinal and intraretinal hemorrhages in the absence of retinal/choroidal lesions, diagnosed with infective endocarditis (IE).
CASE SUMMARY
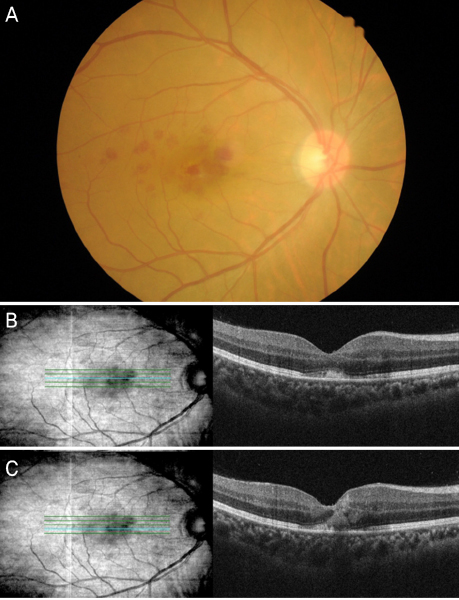
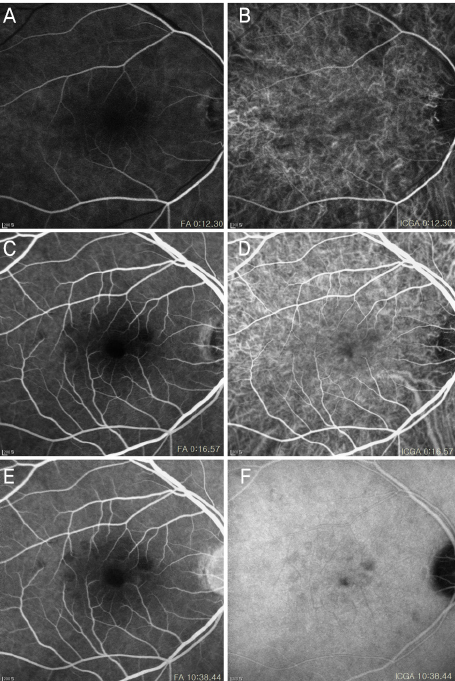
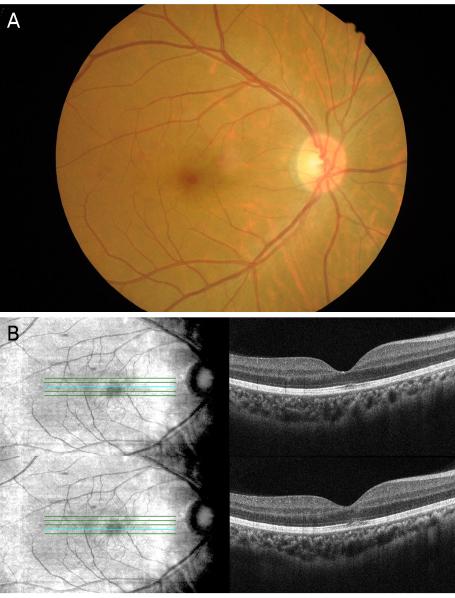
We describe the case of a 44-year-old male with an acute decrease of vision in his right eye. Ophthalmic evaluation revealed multiple subretinal and intraretinal hemorrhages, but no choroidal or other retinal lesions. A systemic examination revealed a pansystolic murmur and blood cultures with echocardiography were suggestive of IE.
CONCLUSIONS
Thorough systemic evaluations are important when patients present with subretinal and intraretinal hemorrhages in the absence of other retinal/choroidal lesions.
MeSH Terms
Figure
Reference
-
1. Hochman MA, Seery CM, Zarbin MA. Pathophysiology and management of subretinal hemorrhage. Surv Ophthalmol. 1997; 42:195–213.2. Silverman ME, Upshaw CB. Extracardiac manifestations of infective endocarditis andtheir historical descriptions. Am J Cardiol. 2007; 100:1802–1807.3. Walpot J, Klazen C, Blok W, van Zwienen J. Embolic events in infective endocarditis: a review and report of 4 cases. Acta Clin Belg. 2005; 60:139–145.4. Sandhya V, Shafquat S. Choroidal neovascularization (CNV) secondary to septic emboli from endocarditis: a case report. Eye (Lond). 2005; 19:822–823.5. Ling R, James B. White-centred retinal haemorrhages (Roth spots). Postgrad Med J. 1998; 74:581–582.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Infective Endocarditis Complicated with Multiple Myocotic Aneurysm and Mitral Valve Perforation
- Systemic Lupus Erythematosus with Purtscher-Like Retinopathy as the First Symptom
- Macroaneurysms of Retinal Arteries
- Neurologic Complications of Infective Endocarditis:Retrospective Review of 100 Cases
- A case of Libman-Sacks endocarditis confused with infective endocarditis