Korean J Sports Med.
2017 Dec;35(3):162-171. 10.5763/kjsm.2017.35.3.162.
Posterior Glenoid Lesions on Magnetic Resonance Imaging in Adolescent Baseball Players
- Affiliations
-
- 1Department of Orthopaedic Surgery, Good Samsun Hospital, Busan, Korea. hongiroom@naver.com
- 2Department of Radiology, Good Samsun Hospital, Busan, Korea.
- KMID: 2397811
- DOI: http://doi.org/10.5763/kjsm.2017.35.3.162
Abstract
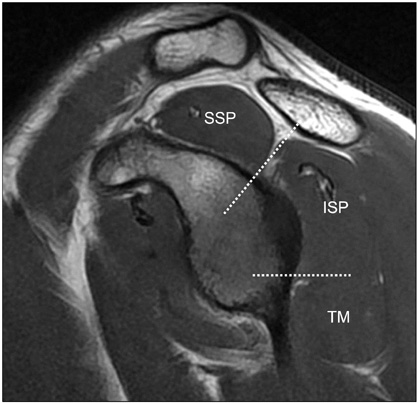
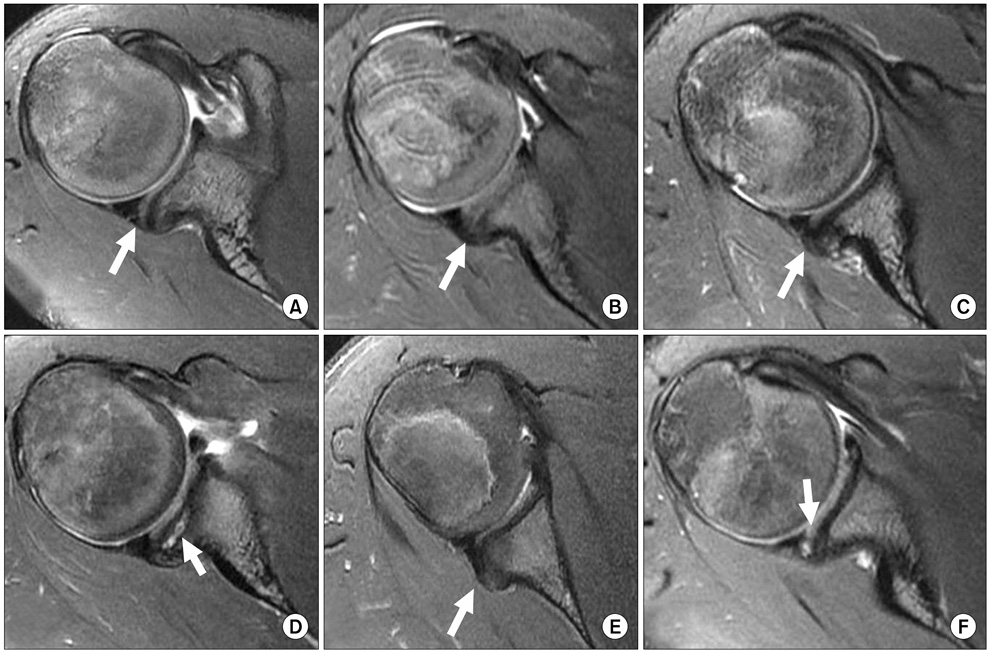
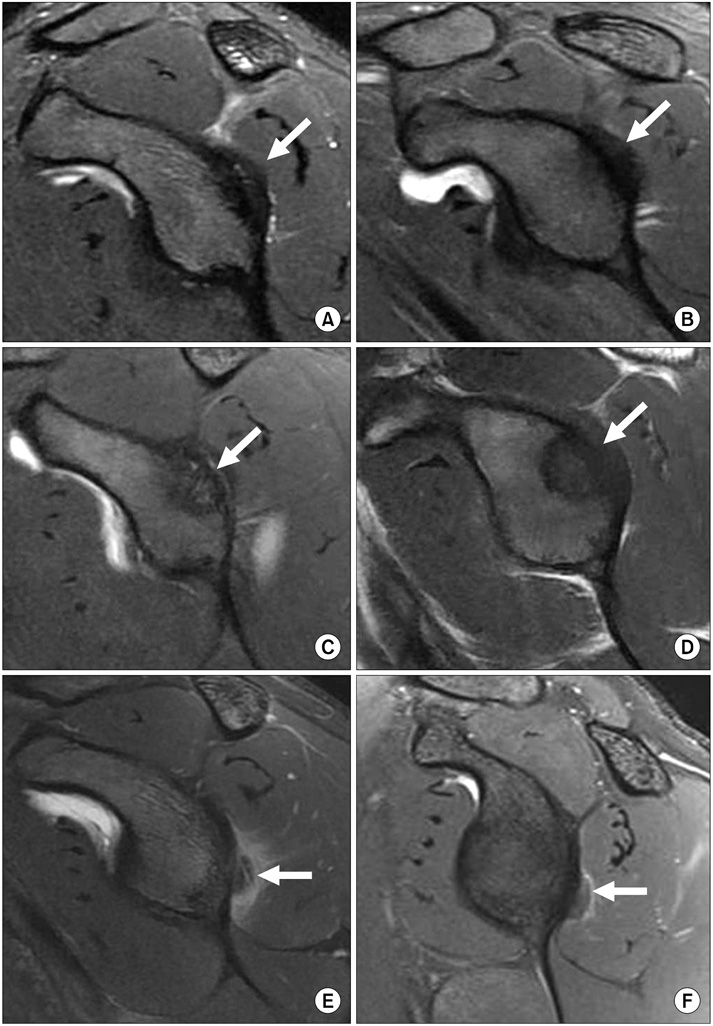
- The purpose of this study is to evaluate the characteristics of posterior glenoid lesion (PGL) on magnetic resonance imaging (MRI) in adolescent baseball players. Seventy-two adolescent baseball players (mean age, 15.1 years) who underwent MRI scan for dominant shoulder pain were enrolled and the location and morphologic features of PGLs were assessed on MRI. All players were divided into three groups based on the physeal status of proximal humerus: group I, open; group II, partial closure; and group III, complete closure. Of the 72 players, posterior glenoid rim rounding (69%) and periosteal thickening (88%) were the main PGL on axial imaging. Osteochondritis dissecans (OCD) of glenoid (10%), Bennett lesion (6%), and posterior labral tear (21%) were also identified. On oblique sagittal imaging, bony PGL including OCD involves mid-portion of posterior glenoid consistent with the level of the infraspinatus muscle, but Bennett lesion was located relatively lower than PGL. Posterior glenoid rim rounding was more prevalent in younger players (group I, 86%; group II, 78%; group III, 43%; p=0.015), and posterior labral tears were in older players (group I, 0%; group II, 19%; group III, 38%, p=0.027). Factors related with prevalence of posterior glenoid rim rounding were increased body mass index (p=0.016), pitchers (p=0.024), and players with posterior shoulder tightness (p=0.023), but career length was not statistically significant (p=0.089). Decreasing the rate of posterior glenoid rim rounding with skeletal growth implies that it may be recovered through the remodeling process, and labral tears are increasing internal impingement lesion after physeal closure.
MeSH Terms
Figure
Reference
-
1. Mariscalco MW, Saluan P. Upper extremity injuries in the adolescent athlete. Sports Med Arthrosc. 2011; 19:17–26.2. Lyman S, Fleisig GS, Waterbor JW, et al. Longitudinal study of elbow and shoulder pain in youth baseball pitchers. Med Sci Sports Exerc. 2001; 33:1803–1810.3. Walch G, Boileau P, Noel E, Donell ST. Impingement of the deep surface of the supraspinatus tendon on the posterosuperior glenoid rim: an arthroscopic study. J Shoulder Elbow Surg. 1992; 1:238–245.4. Burkhart SS, Morgan CD, Kibler WB. The disabled throwing shoulder: spectrum of pathology. Part I: pathoanatomy and biomechanics. Arthroscopy. 2003; 19:404–420.5. Sabick MB, Kim YK, Torry MR, Keirns MA, Hawkins RJ. Biomechanics of the shoulder in youth baseball pitchers: implications for the development of proximal humeral epiphysiolysis and humeral retrotorsion. Am J Sports Med. 2005; 33:1716–1722.6. Yamamoto N, Itoi E, Minagawa H, et al. Why is the humeral retroversion of throwing athletes greater in dominant shoulders than in nondominant shoulders? J Shoulder Elbow Surg. 2006; 15:571–575.7. Gusmer PB, Potter HG, Schatz JA, et al. Labral injuries: accuracy of detection with unenhanced MR imaging of the shoulder. Radiology. 1996; 200:519–524.8. Pappas AM, Zawacki RM, McCarthy CF. Rehabilitation of the pitching shoulder. Am J Sports Med. 1985; 13:223–235.9. Erol OB, Bayramoglu Z, Ertem F, Sharifov R, Yilmaz R, Yekeler E. Forensic age estimation according to fusion of proximal humeral epiphysis in 1367 living Turkish subjects' radiographs: a preliminary study. Austin J Forensic Sci Criminol. 2016; 3:1050.10. Cardoso HF. Age estimation of adolescent and young adult male and female skeletons II, epiphyseal union at the upper limb and scapular girdle in a modern Portuguese skeletal sample. Am J Phys Anthropol. 2008; 137:97–105.11. Mithofer K, Fealy S, Altchek DW. Arthroscopic treatment of internal impingement of the shoulder. Tech Shoulder Elb Surg. 2004; 5:66–75.12. Drakos MC, Rudzki JR, Allen AA, Potter HG, Altchek DW. Internal impingement of the shoulder in the overhead athlete. J Bone Joint Surg Am. 2009; 91:2719–2728.13. Levitz CL, Dugas J, Andrews JR. The use of arthroscopic thermal capsulorrhaphy to treat internal impingement in baseball players. Arthroscopy. 2001; 17:573–577.14. Thomas SJ, Swanik CB, Kaminski TW, et al. Humeral retroversion and its association with posterior capsule thickness in collegiate baseball players. J Shoulder Elbow Surg. 2012; 21:910–916.15. Weishaupt D, Zanetti M, Nyffeler RW, Gerber C, Hodler J. Posterior glenoid rim deficiency in recurrent (atraumatic) posterior shoulder instability. Skeletal Radiol. 2000; 29:204–210.16. Lombardo SJ, Jobe FW, Kerlan RK, Carter VS, Shields CL Jr. Posterior shoulder lesions in throwing athletes. Am J Sports Med. 1977; 5:106–110.17. Zlatkin MB, Sanders TG. Magnetic resonance imaging of the glenoid labrum. Radiol Clin North Am. 2013; 51:279–297.18. Bennett GE. Shoulder and elbow lesions of the professional baseball pitcher. JAMA. 1941; 117:510–514.19. Miniaci A, Mascia AT, Salonen DC, Becker EJ. Magnetic resonance imaging of the shoulder in asymptomatic professional baseball pitchers. Am J Sports Med. 2002; 30:66–73.20. Park JY, Noh YM, Chung SW, et al. Bennett lesions in baseball players detected by magnetic resonance imaging: assessment of association factors. J Shoulder Elbow Surg. 2016; 25:730–738.21. Gogus A, Ozturk C. Osteochondritis dissecans of the glenoid cavity: a case report. Arch Orthop Trauma Surg. 2008; 128:457–460.22. Grau LC, Jose J, Sama AJ, Baraga MG. Osteochondritis dissecans of the glenoid in a major league baseball prospect: a case report. JBJS Case Connector. 2016; 6:e100.23. Han KJ, Kim YK, Lim SK, Park JY, Oh KS. The effect of physical characteristics and field position on the shoulder and elbow injuries of 490 baseball players: confirmation of diagnosis by magnetic resonance imaging. Clin J Sport Med. 2009; 19:271–276.24. Krajnik S, Fogarty KJ, Yard EE, Comstock RD. Shoulder injuries in US high school baseball and softball athletes, 2005-2008. Pediatrics. 2010; 125:497–501.25. Zaremski JL, Krabak BJ. Shoulder injuries in the skeletally immature baseball pitcher and recommendations for the prevention of injury. PM R. 2012; 4:509–516.26. Nakagawa S, Yoneda M, Hayashida K, Mizuno N, Yamada S. Posterior shoulder pain in throwing athletes with a Bennett lesion: factors that influence throwing pain. J Shoulder Elbow Surg. 2006; 15:72–77.27. Ku JH, Cho HL, Jin HK, Park KB, Shin MJ. Ultrasonographic findings of little leaguer's shoulder. Korean J Sports Med. 2016; 34:132–138.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Osseous Erosion by Spinoglenoid Ganglion Cyst in Adolescent Baseball Player: A Case Report
- Upper Extremity Injuries in Youth Baseball Players
- Does Well Maintained Graft Provide Consistent Return to Play after Medial Ulnar Collateral Ligament Reconstruction of the Elbow Joint in Elite Baseball Players?
- Early Lateral Compartment Physeal Closure of the Elbow in Osteochondritis Dissecans of the Adolescent Baseball Players
- Baseball Player's Elbow in Adolescents