Ann Hepatobiliary Pancreat Surg.
2017 Nov;21(4):217-222. 10.14701/ahbps.2017.21.4.217.
Totally laparoscopic associating liver partition and portal vein ligation for staged hepatectomy using anterior approach in HCC patient with Type II portal vein anomaly: a case report
- Affiliations
-
- 1Department of Surgery, Kyungpook National University Hospital, Kyungpook National University School of Medicine, Daegu, Korea. gshys@knu.ac.kr
- KMID: 2397802
- DOI: http://doi.org/10.14701/ahbps.2017.21.4.217
Abstract
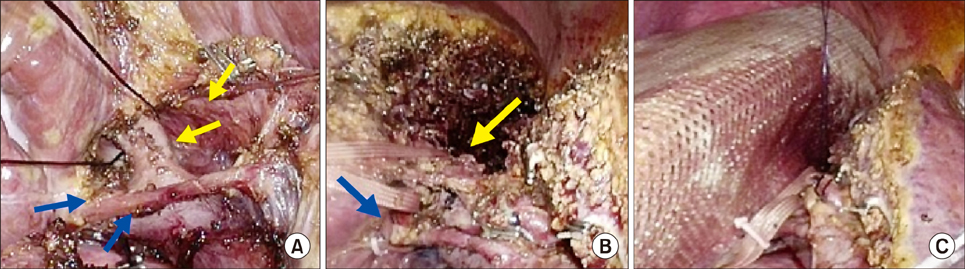
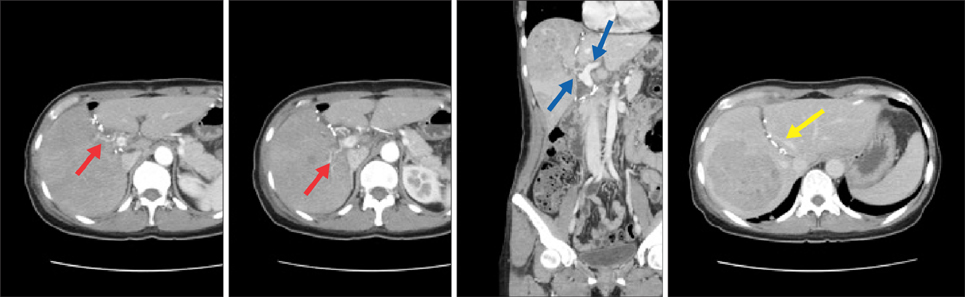
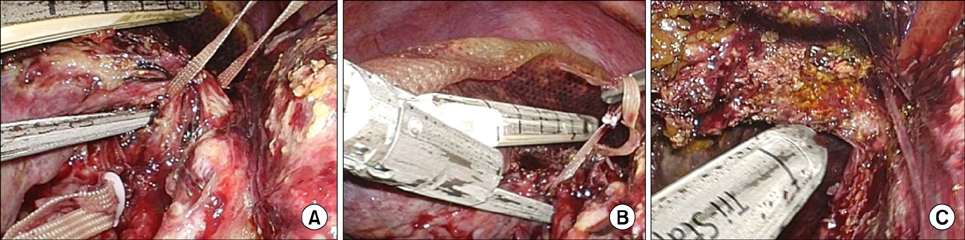
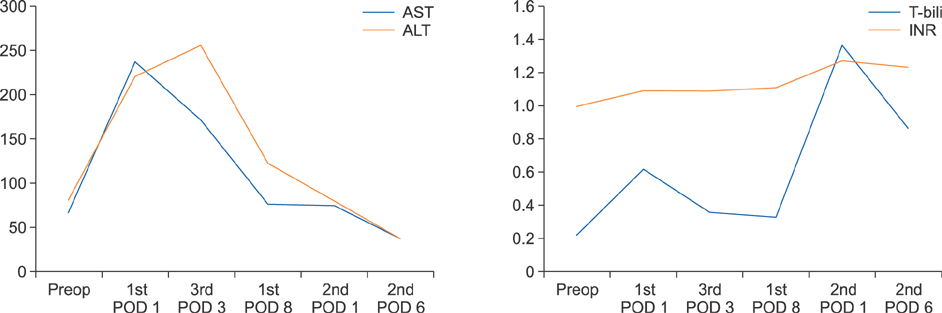
- Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) has gradually developed because of rapid hypertrophy of the future liver remnant volume (FLR) in spite of high morbidity. To minimize the patient's postoperative pain and morbidity including wound complication caused by two consecutive major abdominal operations, we adopted a totally laparoscopic approach and used a composite mesh graft. Also, to maximize the oncologic efficacy, we adopted the "anterior approach" technique. A 44-year-old woman with large hepatitis B-related hepatocellular carcinoma (HCC) in her right lobe was transferred to our hospital for surgical treatment. Preoperatively predicted FLR by a CT scan was 21% and type II portal vein anomaly was detected. A totally laparoscopic approach was planned. During the first stage operation, right anterior and posterior portal veins were meticulously dissected and tied. After parenchymal transection by the "anterior approach" technique, two glissonian pedicles of the right liver were individually isolated. A composite mesh graft was used to prevent severe adhesion on both liver partition surfaces. During the second-stage operation, 9 days after the first stage operation, the two isolated glissonian pedicles were initially transected. After full mobilization of the right lobe, the right hepatic vein was also transected. The right lobe was removed through the Pfannenstiel incision. She was discharged 7 days after the second stage operation. Her postoperative course was uneventful and there was no HCC recurrence for 15 months after hepatectomy. A totally laparoscopic ALPPS procedure can be a feasible technique that ensures patient safety and oncologic superiority, even in patients with complicated anatomical variation.
Keyword
MeSH Terms
Figure
Reference
-
1. Kishi Y, Abdalla EK, Chun YS, Zorzi D, Madoff DC, Wallace MJ, et al. Three hundred and one consecutive extended right hepatectomies: evaluation of outcome based on systematic liver volumetry. Ann Surg. 2009; 250:540–548.2. Hemming AW, Reed AI, Howard RJ, Fujita S, Hochwald SN, Caridi JG, et al. Preoperative portal vein embolization for extended hepatectomy. Ann Surg. 2003; 237:686–693.3. Liu H, Zhu S. Present status and future perspectives of preoperative portal vein embolization. Am J Surg. 2009; 197:686–690.4. Schadde E, Malagó M, Hernandez-Alejandro R, Li J, Abdalla E, Ardiles V, et al. Monosegment ALPPS hepatectomy: extending resectability by rapid hypertrophy. Surgery. 2015; 157:676–689.5. Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, Farkas SA, et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg. 2012; 255:405–414.6. Burpee SE, Kurian M, Murakame Y, Benevides S, Gagner M. The metabolic and immune response to laparoscopic versus open liver resection. Surg Endosc. 2002; 16:899–904.7. Machado MA, Makdissi FF, Surjan RC. Totally laparoscopic ALPPS is feasible and may be worthwhile. Ann Surg. 2012; 256:e13.8. Cho A, Yamamoto H, Kainuma O, Ota T, Park S, Arimitsu H, et al. Extrahepatic Glissonean approach for laparoscopic major liver resection (with video). J Hepatobiliary Pancreat Sci. 2013; 20:141–144.9. Sureka B, Patidar Y, Bansal K, Rajesh S, Agrawal N, Arora A. Portal vein variations in 1000 patients: surgical and radiological importance. Br J Radiol. 2015; 88:20150326.10. Jaeck D, Oussoultzoglou E, Rosso E, Greget M, Weber JC, Bachellier P. A two-stage hepatectomy procedure combined with portal vein embolization to achieve curative resection for initially unresectable multiple and bilobar colorectal liver metastases. Ann Surg. 2004; 240:1037–1049.11. Broering DC, Hillert C, Krupski G, Fischer L, Mueller L, Achilles EG, et al. Portal vein embolization vs. portal vein ligation for induction of hypertrophy of the future liver remnant. J Gastrointest Surg. 2002; 6:905–913.12. de Santibañes E, Clavien PA. Playing Play-Doh to prevent postoperative liver failure: the “ALPPS” approach. Ann Surg. 2012; 255:415–417.13. de Santibañes E, Alvarez FA, Ardiles V. How to avoid postoperative liver failure: a novel method. World J Surg. 2012; 36:125–128.14. Adam R, Laurent A, Azoulay D, Castaing D, Bismuth H. Two-stage hepatectomy: a planned strategy to treat irresectable liver tumors. Ann Surg. 2000; 232:777–785.15. Alvarez FA, Iniesta J, Lastiri J, Ulla M, Bonadeo Lassalle F, de Santibañes E. New method of hepatic regeneration. Cir Esp. 2011; 89:645–649.16. Aloia TA, Vauthey JN. Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): what is gained and what is lost? Ann Surg. 2012; 256:e9.17. Dokmak S, Rasoaherinomenjanahary F, Cauchy F, Aussilhou B, Belghiti J. Does ALPPS regularly increase the future remnant liver and prevent postoperative liver failure? HPB (Oxford). 2014; 16:Suppl 2. 169.18. Schadde E, Ardiles V, Robles-Campos R, Malago M, Machado M, Hernandez-Alejandro R, et al. Early survival and safety of ALPPS: first report of the International ALPPS Registry. Ann Surg. 2014; 260:829–838.19. Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg. 2015; 261:619–629.20. Machado MA, Makdissi FF, Surjan RC, Basseres T, Schadde E. Transition from open to laparoscopic ALPPS for patients with very small FLR: the initial experience. HPB (Oxford). 2017; 19:59–66.21. Zhang Y, Yang H, Chen Y, Zhu S, Lu T, Jun X. Totally laparoscopic associating liver tourniquet and portal ligation for staged hepatectomy via anterior approach for cirrhotic hepatocellular carcinoma. J Am Coll Surg. 2015; 221:e43–e48.22. Xiao L, Li JW, Zheng SG. Totally laparoscopic ALPPS in the treatment of cirrhotic hepatocellular carcinoma. Surg Endosc. 2015; 29:2800–2801.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Associating microwave ablation and portal vein ligation for staged hepatectomy for the treatment of huge hepatocellular carcinoma with cirrhosis
- Monosegment associating liver partition and portal vein ligation for staged hepatectomy: Preserving segment 1 as the only liver remnant after hepatocellular carcinoma recurrence
- Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS) procedure for hepatocellular carcinoma with chronic liver disease: a case report and review of literature
- Portal vein fenestration: a case report of an unusual portal vein developmental anomaly
- Surgical management of hilar cholangiocarcinoma: Controversies and recommendations