A Prospective Survey of Atrial Fibrillation Management for Real-world Guideline Adherence: COmparison study of Drugs for symptom control and complication prEvention of Atrial Fibrillation (CODE-AF) Registry
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. cby6908@yuhs.ac
- 2Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea.
- 3Division of Cardiology, Department of Internal Medicine, Kyung Hee University Hospital, Kyung Hee University, Seoul, Korea.
- 4Department of Cardiology, School of Medicine, Ewha Womans University, Seoul, Korea.
- 5Department of Cardiology, Hanyang University Seoul Hospital, Seoul, Korea.
- 6Division of Cardiology, Eulji University Hospital, Daejeon, Korea.
- 7Division of Cardiology, Department of Internal Medicine, Korea University Medical Center, Seoul, Korea.
- 8Heart Institute, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea.
- 9Department of Cardiology, Chonnam National University Hospital, Chonnam National University School of Medicine, Gwangju, Korea.
- 10Department of Preventive Medicine, Institute of Human Complexity and Systems Science, Yonsei University College of Medicine, Seoul, Korea.
- 11Division of Cardiology, Department of Internal Medicine, Daegu Catholic University Medical Center, Catholic University of Daegu, Daegu, Korea. mdleeys@cu.ac.kr
- KMID: 2396481
- DOI: http://doi.org/10.4070/kcj.2017.0146
Abstract
- BACKGROUND AND OBJECTIVES
The aging population is rapidly increasing, and atrial fibrillation (AF) is becoming a significant public health burden in Asia, including Korea. This study evaluated current treatment patterns and guideline adherence of AF treatment.
METHODS
In a prospective observational registry (COmparison study of Drugs for symptom control and complication prEvention of Atrial Fibrillation [CODE-AF] registry), 6,275 patients with nonvalvular AF were consecutively enrolled between June 2016 and April 2017 from 10 tertiary hospitals in Korea.
RESULTS
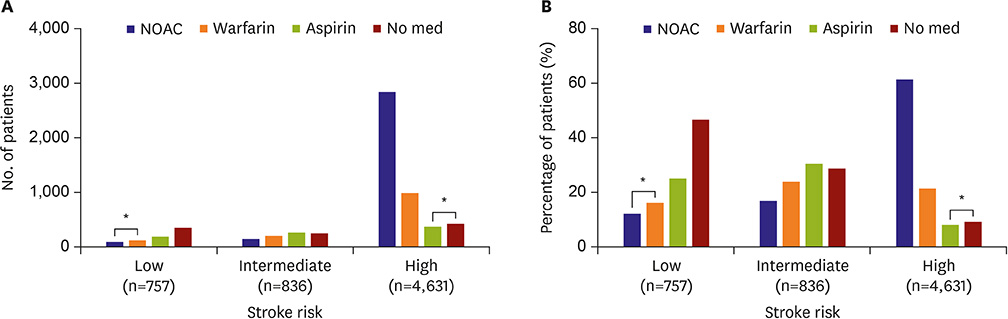
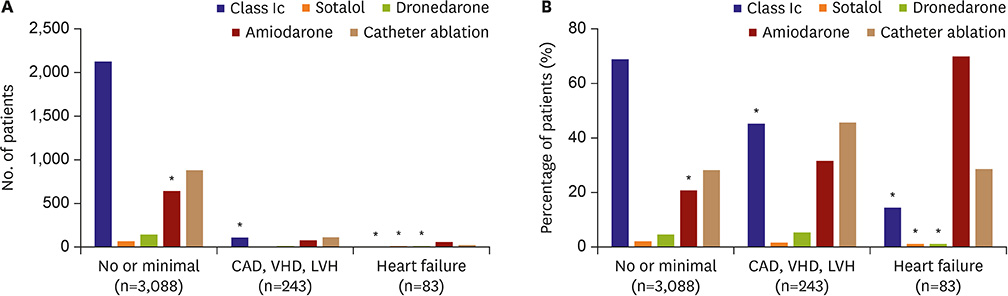
The AF type was paroxysmal, persistent, and permanent in 65.3%, 30.0%, and 2.9% of patients, respectively. Underlying structural heart disease was present in 11.9%. Mean CHA2DS2-VASc was 2.7±1.7. Oral anticoagulation (OAC), rate control, and rhythm control were used in 70.1%, 53.9%, and 54.4% of patients, respectively. OAC was performed in 82.7% of patients with a high stroke risk. However, antithrombotic therapy was inadequately used in 53.4% of patients with a low stroke risk. For rate control in 192 patients with low ejection fraction (< 40%), β-blocker (65.6%), digoxin (5.2%), or both (19.3%) were adequately used in 90.1% of patients; however, a calcium channel blocker was inadequately used in 9.9%. A rhythm control strategy was chosen in 54.4% of patients. The prescribing rate of class Ic antiarrythmics, dronedarone, and sotalol was 16.9% of patients with low ejection fraction.
CONCLUSION
This study shows how successfully guidelines can be applied in the real world. The nonadherence rate was 17.2%, 9.9%, and 22.4% for stroke prevention, rate control, and rhythm control, respectively.
MeSH Terms
Figure
Cited by 9 articles
-
2018 Korean Guideline of Atrial Fibrillation Management
Boyoung Joung, Jung Myung Lee, Ki Hong Lee, Tae-Hoon Kim, Eue-Keun Choi, Woo-Hyun Lim, Ki-Woon Kang, Jaemin Shim, Hong Euy Lim, Junbeom Park, So-Ryoung Lee, Young Soo Lee, Jin-Bae Kim,
Korean Circ J. 2018;48(12):1033-1080. doi: 10.4070/kcj.2018.0339.Regional and Socioeconomic Inequality of Atrial Fibrillation with Regular Hospital Visit
Pil-Sung Yang, Boyoung Joung
Korean Circ J. 2018;48(7):635-636. doi: 10.4070/kcj.2018.0116.Stroke Prevention in Atrial Fibrillation: Focus on Asian Patients
Yan-Guang Li, So-Ryoung Lee, Eue-Keun Choi, Gregory Y.H. Lip
Korean Circ J. 2018;48(8):665-684. doi: 10.4070/kcj.2018.0190.Social Inequalities of Oral Anticoagulation after the Introduction of Non-Vitamin K Antagonists in Patients with Atrial Fibrillation
Hee Tae Yu, Pil-Sung Yang, Jinseub Hwang, Soorack Ryu, Eunsun Jang, Tae-Hoon Kim, Jae-Sun Uhm, Jong-Youn Kim, Hui-Nam Pak, Moon-Hyoung Lee, Gregory Y.H. Lip, Boyoung Joung
Korean Circ J. 2020;50(3):267-277. doi: 10.4070/kcj.2019.0207.Comparison of Rhythm and Rate Control Strategies for Stroke Occurrence in a Prospective Cohort of Atrial Fibrillation Patients
Yu Jeong Choi, Ki-Woon Kang, Tae-Hoon Kim, Myung-Jin Cha, Jung-Myung Lee, Junbeom Park, Jin-Kyu Park, Jaemin Shim, Jae-Sun Uhm, Jun Kim, Hyung Wook Park, Eue-Keun Choi, Jin-Bae Kim, Changsoo Kim, Young Soo Lee, Boyoung Joung
Yonsei Med J. 2018;59(2):258-264. doi: 10.3349/ymj.2018.59.2.258.Label Adherence for Non-Vitamin K Antagonist Oral Anticoagulants in a Prospective Cohort of Asian Patients with Atrial Fibrillation
So-Ryoung Lee, Young Soo Lee, Ji-Suck Park, Myung-Jin Cha, Tae-Hoon Kim, Junbeom Park, Jin-Kyu Park, Jung-Myung Lee, Ki-Woon Kang, Jaemin Shim, Jae-Sun Uhm, Jun Kim, Changsoo Kim, Jin-Bae Kim, Hyung Wook Park, Boyoung Joung, Eue-Keun Choi
Yonsei Med J. 2019;60(3):277-284. doi: 10.3349/ymj.2019.60.3.277.Antithrombotic Medication and the Risk of Vitreous Hemorrhage in Atrial Fibrillation: Korean National Health Insurance Service National Cohort
Ko Eun Kim, Pil-Sung Yang, Eunsun Jang, Sungjin Kim, Boyoung Joung
Yonsei Med J. 2019;60(1):65-72. doi: 10.3349/ymj.2019.60.1.65.Current Anticoagulant Usage Patterns and Determinants in Korean Patients with Nonvalvular Atrial Fibrillation
Hyun Su Ha, Joongmin Kim, Young Soo Lee, Tae-Hoon Kim, Jung Myung Lee, Junbeom Park, Jin-Kyu Park, Ki-Woon Kang, Jaemin Shim, Jae-Sun Uhm, Hyung Wook Park, Myung-Jin Cha, Eue-Keun Choi, Jun Kim, Jin-Bae Kim, Changsoo Kim, Boyoung Joung
Yonsei Med J. 2020;61(2):120-128. doi: 10.3349/ymj.2020.61.2.120.Association of Gender With Clinical Outcomes in a Contemporary Cohort of Patients With Atrial Fibrillation Receiving Oral Anticoagulants
Minjeong Kim, Jun Kim, Jin-Bae Kim, Junbeom Park, Jin-Kyu Park, Ki-Woon Kang, Jaemin Shim, Eue-Keun Choi, Young Soo Lee, Hyung Wook Park, Boyoung Joung
Korean Circ J. 2022;52(8):593-603. doi: 10.4070/kcj.2021.0399.
Reference
-
1. Lee H, Kim TH, Baek YS, et al. The trends of atrial fibrillation-related hospital visit and cost, treatment pattern and mortality in Korea: 10-year nationwide sample cohort data. Korean Circ J. 2017; 47:56–64.2. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014; 130:e199–e267.3. Park J, Park CH, Uhm JS, Pak HN, Lee MH, Joung B. A thin left atrial antral wall around the pulmonary vein reflects structural remodeling by atrial fibrillation and is associated with stroke. Yonsei Med J. 2017; 58:282–289.4. Kim TH, Yang PS, Uhm JS, et al. Cha2ds2-vasc score (congestive heart failure, hypertension, age ≥75 [doubled], diabetes mellitus, prior stroke or transient ischemic attack [doubled], vascular disease, age 65–74, female) for stroke in Asian patients with atrial fibrillation: a Korean nationwide sample cohort study. Stroke. 2017; 48:1524–1530.5. Lip GY, Al-Khatib SM, Cosio FG, et al. Contemporary management of atrial fibrillation: what can clinical registries tell us about stroke prevention and current therapeutic approaches? J Am Heart Assoc. 2014; 3:e001179.6. Hart RG, Pearce LA, Aguilar MI. Adjusted-dose warfarin versus aspirin for preventing stroke in patients with atrial fibrillation. Ann Intern Med. 2007; 147:590–592.7. Gorst-Rasmussen A, Skjøth F, Larsen TB, Rasmussen LH, Lip GY, Lane DA. Dabigatran adherence in atrial fibrillation patients during the first year after diagnosis: a nationwide cohort study. J Thromb Haemost. 2015; 13:495–504.8. Donzé J, Clair C, Hug B, et al. Risk of falls and major bleeds in patients on oral anticoagulation therapy. Am J Med. 2012; 125:773–778.9. Al-Khatib SM, Allen LaPointe NM, Chatterjee R, et al. Rate- and rhythm-control therapies in patients with atrial fibrillation: a systematic review. Ann Intern Med. 2014; 160:760–773.10. Nikolaidou T, Channer KS. Chronic atrial fibrillation: a systematic review of medical heart rate control management. Postgrad Med J. 2009; 85:303–312.11. Lafuente-Lafuente C, Mouly S, Longas-Tejero MA, Bergmann JF. Antiarrhythmics for maintaining sinus rhythm after cardioversion of atrial fibrillation. Cochrane Database Syst Rev. 2007; CD005049.12. Anselmino M, Matta M, D'Ascenzo F, et al. Catheter ablation of atrial fibrillation in patients with left ventricular systolic dysfunction: a systematic review and meta-analysis. Circ Arrhythm Electrophysiol. 2014; 7:1011–1018.13. Cosedis Nielsen J, Johannessen A, Raatikainen P, et al. Radiofrequency ablation as initial therapy in paroxysmal atrial fibrillation. N Engl J Med. 2012; 367:1587–1595.14. Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016; 37:2893–2962.15. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014; 130:2071–2104.16. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College Of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014; 64:e1–76.17. Huisman MV, Ma CS, Diener HC, et al. Antithrombotic therapy use in patients with atrial fibrillation before the era of non-vitamin K antagonist oral anticoagulants: the Global Registry on Long-term Oral Antithrombotic Treatment in Patients with Atrial Fibrillation (GLORIA-AF) Phase I cohort. Europace. 2016; 18:1308–1318.18. Huisman MV, Rothman KJ, Paquette M, et al. The changing landscape for stroke prevention in AF: findings from the GLORIA-AF Registry Phase 2. J Am Coll Cardiol. 2017; 69:777–785.19. Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009; 361:1139–1151.20. Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011; 365:883–891.21. Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011; 365:981–992.22. Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013; 369:2093–2104.23. Chao TF, Wang KL, Liu CJ, et al. Age threshold for increased stroke risk among patients with atrial fibrillation: a nationwide cohort study from Taiwan. J Am Coll Cardiol. 2015; 66:1339–1347.24. Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007; 146:857–867.25. Birman-Deych E, Radford MJ, Nilasena DS, Gage BF. Use and effectiveness of warfarin in medicare beneficiaries with atrial fibrillation. Stroke. 2006; 37:1070–1074.26. Indredavik B, Rohweder G, Lydersen S. Frequency and effect of optimal anticoagulation before onset of ischaemic stroke in patients with known atrial fibrillation. J Intern Med. 2005; 258:133–144.27. Sandhu RK, Bakal JA, Ezekowitz JA, McAlister FA. Risk stratification schemes, anticoagulation use and outcomes: the risk--treatment paradox in patients with newly diagnosed non-valvular atrial fibrillation. Heart. 2011; 97:2046–2050.28. Van Gelder IC, Groenveld HF, Crijns HJ, et al. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010; 362:1363–1373.29. Piccini JP, Mi X, DeWald TA, Go AS, Hernandez AF, Curtis LH. Pharmacotherapy in Medicare beneficiaries with atrial fibrillation. Heart Rhythm. 2012; 9:1403–1408.30. Le Heuzey JY, Breithardt G, Camm J, et al. The RecordAF study: design, baseline data, and profile of patients according to chosen treatment strategy for atrial fibrillation. Am J Cardiol. 2010; 105:687–693.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Guideline of atrial fibrillation management
- A prospective survey of the persistence of warfarin or NOAC in nonvalvular atrial fibrillation: a COmparison study of Drugs for symptom control and complication prEvention of Atrial Fibrillation (CODE-AF)
- Pharmacological Treatment of Atrial Fibrillation
- Nonpharmacologic Treatment for Atrial Fibrillation
- The Joint Multicenter Study on the Atrial Fibrillation in Korea