Current Status and Future of Lung Donation in Korea
- Affiliations
-
- 1Department of Pulmonology and Critical Care Medicine, Pusan National University Yangsan Hospital, Yangsan, Korea. yumccs@nate.com
- 2Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea. yumccs@nate.com
- 3Department of Thoracic and Cardiovascular Surgery, Pusan National University Yangsan Hospital, Yangsan, Korea.
- KMID: 2396371
- DOI: http://doi.org/10.3346/jkms.2017.32.12.1953
Abstract
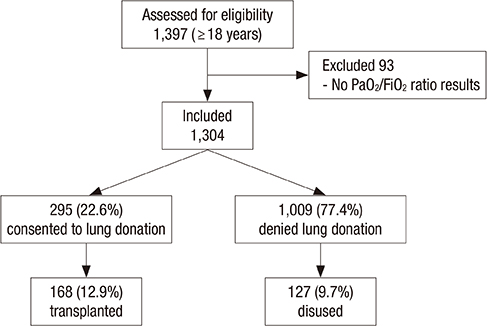
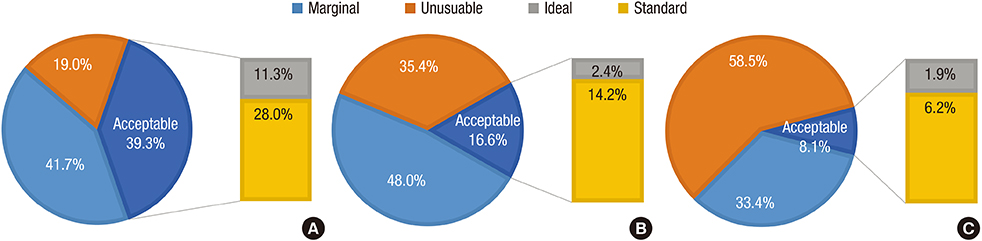
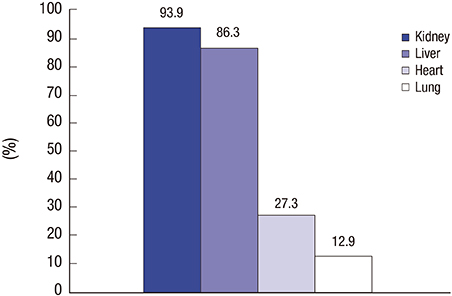
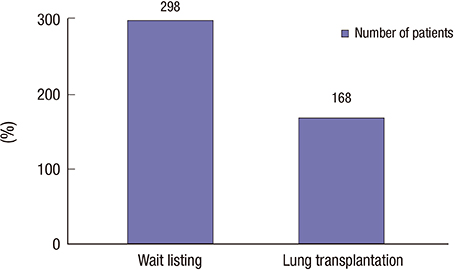
- Lung transplantation is the only effective treatment option for patients with end-stage lung disease. However, donor organ shortage makes timely transplant not possible for all patients, especially in Korea. We investigated the number and utilization of donor lungs by retrospectively reviewing all donor organs registered in the Korea Network for Organ Sharing database from March 2012 to March 2016. The donors were stratified into 4 groups by donor acceptability criteria. A total of 1,304 donors were included. Of those, 295 brain-dead donors (22.6%) consented to lung donation. Among these consented donors, 168 donors (12.9%) were retrieved for lung transplant. Retrieval rate was very low compared with that of the kidney (93.9%), liver (86.3%), and heart (27.3%). The characteristics of utilized donor lungs were: mean age, 40.5 years (range: 18 to 63 years); mean partial pressure of oxygen, 356.5 mmHg; mean smoking history, 5.9 pack-years; and mean body mass index, 22.6 kg/m². The proportion of donors with acceptable condition of the transplanted lungs was only 39.3% (ideal 19, standard 47, marginal 70, unusable 32). Among brain-dead patients who denied to donate lungs (n = 1,009), 82 were potentially acceptable donors (ideal 19, standard 63), which was equal to half of actually transplanted lung donations. Many potential donor lungs, which are currently excluded, may be successfully used in lung transplantation in Korea. The available lung donors must be actively selected and managed to maximize the utilization of this precious resource.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
Impact of extended-criteria donor lungs according to preoperative recipient status and age in lung transplantation
Jee Won Suh, Jin Gu Lee, Moo Suk Park, Song Yee Kim, Su Jin Jeong, Hyo Chae Paik
Korean J Transplant. 2020;34(3):185-192. doi: 10.4285/kjt.2020.34.3.185.Performance Changes Following the Revision of Organ Allocation System of Lung Transplant: Analysis of Korean Network for Organ Sharing Data
Hye Ju Yeo, Do Hyung Kim, Yun Seong Kim, Doosoo Jeon, Woo Hyun Cho
J Korean Med Sci. 2021;36(12):e79. doi: 10.3346/jkms.2021.36.e79.The First Living-Donor Lobar Lung Transplantation in Korea: a Case Report
Sehoon Choi, Seung-Il Park, Geun Dong Lee, Hyeong Ryul Kim, Dong Kwan Kim, Sung-Ho Jung, Tae-Jin Yun, In Ok Kim, Dae-Kee Choi, In-Cheol Choi, Jong-Min Song, Sang-Bum Hong, Tae Sun Shim, Kyung-Wook Jo, Sang-Oh Lee, Kyung-Hyun Do, Eun Jin Chae
J Korean Med Sci. 2018;33(43):. doi: 10.3346/jkms.2018.33.e282.Outcomes of Patients on the Lung Transplantation Waitlist in Korea: A Korean Network for Organ Sharing Data Analysis
Hye Ju Yeo, Dong Kyu Oh, Woo Sik Yu, Sun Mi Choi, Kyeongman Jeon, Mihyang Ha, Jin Gu Lee, Woo Hyun Cho, Young Tae Kim
J Korean Med Sci. 2022;37(41):e294. doi: 10.3346/jkms.2022.37.e294.
Reference
-
1. Korean Network for Organ Sharing. 2015 KONOS annual report [Internet]. accessed on 1 July 2016. Available at https://www.konos.go.kr/konosis/common/bizlogic.jsp.2. Paik HC, Haam SJ, Lee DY, Yi GJ, Song SW, Kim YT, Kang CH, Kim KM, Park SI, Jheon SH. The fate of patients on the waiting list for lung transplantation in Korea. Transplant Proc. 2012; 44:865–869.3. Eurotransplant International Foundation (NL). Annual report 2014 [Internet]. accessed on 16 October 2017. Available at https://www.eurotransplant.org/cms/mediaobject.php?file=ar_2014.pdf.4. United Network for Organ Sharing (US). Annual report 2014 [Internet]. accessed on 16 October 2017. Available at http://www.unos.org/data/data-resources/.5. Kim H, Jeon YK, Lee HJ, Kim YT, Chung DH. Clinico-pathological analysis of the lungs from patients with lung transplantation in a single institute in Korea. J Korean Med Sci. 2015; 30:1439–1445.6. Jhang WK, Park SJ, Lee E, Yang SI, Hong SJ, Seo JH, Kim HY, Park JJ, Yun TJ, Kim HR, et al. The first successful heart-lung transplant in a Korean child with humidifier disinfectant-associated interstitial lung disease. J Korean Med Sci. 2016; 31:817–821.7. Yeo HJ, Lee S, Yoon SH, Lee SE, Cho WH, Jeon D, Kim YS, Kim D. Extracorporeal life support as a bridge to lung transplantation in patients with acute respiratory failure. Transplant Proc. 2017; 49:1430–1435.8. Botha P, Fisher AJ, Dark JH. Marginal lung donors: a diminishing margin of safety? Transplantation. 2006; 82:1273–1279.9. Reyes KG, Mason DP, Thuita L, Nowicki ER, Murthy SC, Pettersson GB, Blackstone EH. Guidelines for donor lung selection: time for revision? Ann Thorac Surg. 2010; 89:1756–1764.10. Yusen RD, Edwards LB, Kucheryavaya AY, Benden C, Dipchand AI, Goldfarb SB, Levvey BJ, Lund LH, Meiser B, Rossano JW, et al. The Registry of the International Society for Heart and Lung Transplantation: thirty-second official adult lung and heart-lung transplantation report--2015; focus theme: early graft failure. J Heart Lung Transplant. 2015; 34:1264–1277.11. NHS Blood and Transplant (US). Organ donation and transplantation activity report 2014/15 [Internet]. accessed on 16 October 2017. Available at http://nhsbtmediaservices.blob.core.windows.net/organ-donation-assets/pdfs/activity_report_2014_15.pdf.12. Organ and Tissue Authority (AU). Australian donation and transplantation activity report 2015 [Internet]. accessed on 16 October 2017. Available at http://www.donatelife.gov.au/sites/default/files/Australian%20Donation%20and%20Transplantation%20Activity%20Report%202015.pdf.13. Jeong JH. Brain and lung: lung injury in patients with brain injury. J Neurocrit Care. 2017; 10:1–6.14. Faropoulos K, Apostolakis E. Brain death and its influence on the lungs of the donor: how is it prevented? Transplant Proc. 2009; 41:4114–4119.15. Wood KE, Becker BN, McCartney JG, D'Alessandro AM, Coursin DB. Care of the potential organ donor. N Engl J Med. 2004; 351:2730–2739.16. Rosendale JD, Chabalewski FL, McBride MA, Garrity ER, Rosengard BR, Delmonico FL, Kauffman HM. Increased transplanted organs from the use of a standardized donor management protocol. Am J Transplant. 2002; 2:761–768.17. Miñambres E, Pérez-Villares JM, Chico-Fernández M, Zabalegui A, Dueñas-Jurado JM, Misis M, Mosteiro F, Rodriguez-Caravaca G, Coll E. Lung donor treatment protocol in brain dead-donors: a multicenter study. J Heart Lung Transplant. 2015; 34:773–780.18. Abuanzeh R, Hashmi F, Dimarakis I, Khasati N, Machaal A, Yonan N, Venkateswaran RV. Early donor management increases the retrieval rate of hearts for transplantation in marginal donors. Eur J Cardiothorac Surg. 2015; 47:72–77.19. NHS Blood and Transplant (US). Donation after brainstem death (DBD): donor optimisation extended care bundle [Internet]. accessed on 16 October 2017. Available at http://odt.nhs.uk/pdf/dbd_care_bundle.pdf.20. Mascia L, Pasero D, Slutsky AS, Arguis MJ, Berardino M, Grasso S, Munari M, Boifava S, Cornara G, Della Corte F, et al. Effect of a lung protective strategy for organ donors on eligibility and availability of lungs for transplantation: a randomized controlled trial. JAMA. 2010; 304:2620–2627.21. Westphal GA, Garcia VD, Souza RL, Franke CA, Vieira KD, Birckholz VR, Machado MC, Almeida ER, Machado FO, Sardinha LA, et al. Guidelines for the assessment and acceptance of potential brain-dead organ donors. Rev Bras Ter Intensiva. 2016; 28:220–255.22. Schiavon M, Falcoz PE, Santelmo N, Massard G. Does the use of extended criteria donors influence early and long-term results of lung transplantation? Interact Cardiovasc Thorac Surg. 2012; 14:183–187.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Donation after Circulatory Death in Lung Transplantation
- The Influence of Plateletpheresis Donors' Attitudes on Their Willingness to Give Future Donations and to Recommend Donation to Others
- Factors Influencing Family's Organ Donation Decision
- Molecular Pathology of Lung Cancer: Current Status and Future Directions
- Current Status of Immunotherapy for Lung Cancer and Future Perspectives