J Korean Neurosurg Soc.
2017 Nov;60(6):755-762. 10.3340/jkns.2017.0606.003.
Lateral Lumbar Interbody Fusion and in Situ Screw Fixation for Rostral Adjacent Segment Stenosis of the Lumbar Spine
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University Hospital, Seoul, Korea. ucallitlove1004@hanmail.net
- 2Department of Neurosurgery, The Armed Forces Capital Hospital, Seongnam, Korea.
- 3Department of Neurosurgery, Seoul National University College of Medicine, Seoul, Korea.
- 4Clinical Research Institute, Seoul National University Hospital, Seoul, Korea.
- 5Department of Brain and Cognitive Sciences, Seoul National University College of Natural Sciences, Seoul, Korea.
- 6Department of Neurosurgery, Seoul National University Boramae Hospital, Seoul, Korea.
- 7Department of Neurosurgery, Gyeongsang National University Changwon Hospital, Changwon, Korea.
- KMID: 2395797
- DOI: http://doi.org/10.3340/jkns.2017.0606.003
Abstract
OBJECTIVE
The purpose of this study is to describe the detailed surgical technique and short-term clinical and radiological outcomes of lateral lumbar interbody fusion (LLIF) and in situ lateral screw fixation using a conventional minimally invasive screw fixation system (MISF) for revision surgery to treat rostral lumbar adjacent segment disease.
METHODS
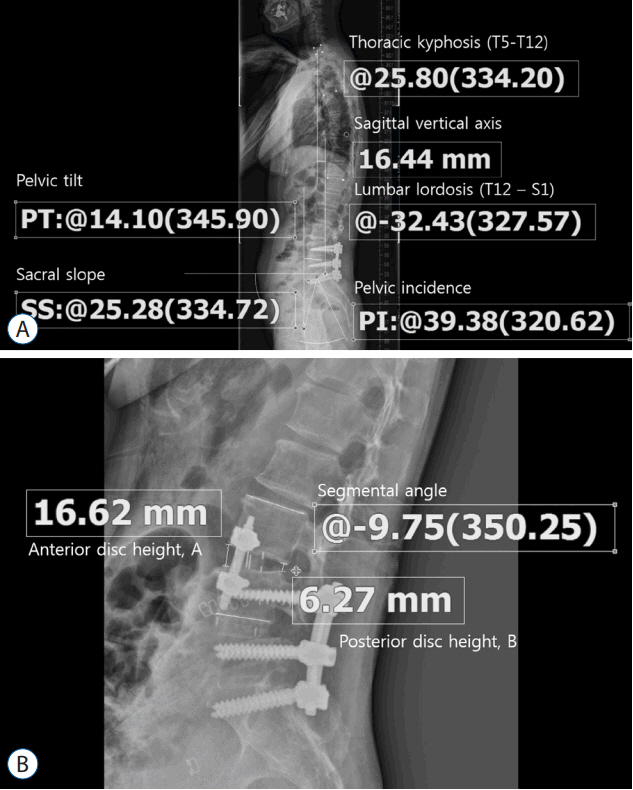
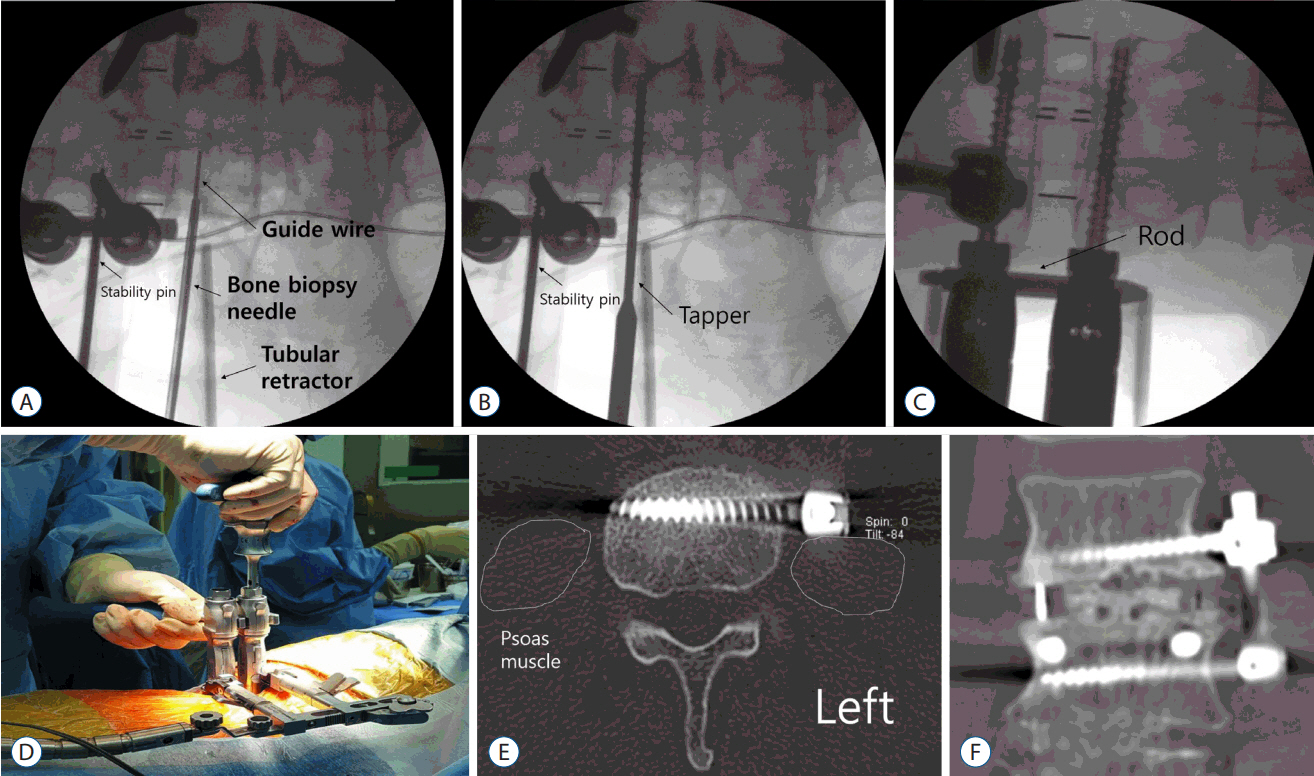
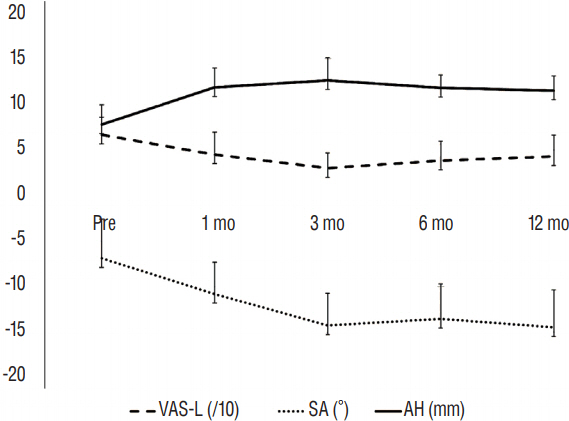
The medical and radiological records were retrospectively reviewed. The surgery was indicated in 10 consecutive patients with rostral adjacent segment stenosis and instability. After the insertion of the interbody cage, lateral screws were inserted into the cranial and caudal vertebra using the MISF through the same LLIF trajectory. The radiological and clinical outcomes were assessed preoperatively and at 1, 3, 6, and 12 months postoperatively.
RESULTS
The median follow-up period was 13 months (range, 3-48 months). Transient sensory changes in the left anterior thigh occurred in 3 patients, and 1 patient experienced subjective weakness; however, these symptoms normalized within 1 week. Back and leg pain were significantly improved (p<0.05). In the radiological analysis, both the segmental angle at the operated segment and anterior disc height were significantly increased. At 6 months postoperatively, solid bony fusion was confirmed in 7 patients. Subsidence and mechanical failure did not occur in any patients.
CONCLUSION
This study demonstrates that LLIF and in situ lateral screw fixation may be an alternative surgical option for rostral lumbar adjacent segment disease.
MeSH Terms
Figure
Reference
-
References
1. Ahmadian A, Bach K, Bolinger B, Malham GM, Okonkwo DO, Kanter AS, et al. Stand-alone minimally invasive lateral lumbar interbody fusion: multicenter clinical outcomes. J Clin Neurosci. 22:740–746. 2015.
Article2. Aiki H, Ohwada O, Kobayashi H, Hayakawa M, Kawaguchi S, Takebayashi T, et al. Adjacent segment stenosis after lumbar fusion requiring second operation. J Orthop Sci. 10:490–495. 2005.
Article3. Barrey C, Jund J, Noseda O, Roussouly P. Sagittal balance of the pelvis-spine complex and lumbar degenerative diseases. A comparative study about 85 cases. Eur Spine J. 16:1459–1467. 2007.
Article4. Bridwell KH, Lenke LG, McEnery KW, Baldus C, Blanke K. Anterior fresh frozen structural allografts in the thoracic and lumbar spine: do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine (Phila Pa 1976). 20:1410–1418. 1995.
Article5. Bridwell KH, Sedgewick TA, O’Brien MF, Lenke LG, Baldus C. The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. J Spinal Disord. 6:461–472. 1993.
Article6. Cheh G, Bridwell KH, Lenke LG, Buchowski JM, Daubs MD, Kim Y, et al. Adjacent segment disease following lumbar/thoracolumbar fusion with pedicle screw instrumentation: a minimum 5-year follow-up. Spine (Phila Pa 1976). 32:2253–2257. 2007.
Article7. Chen WJ, Lai PL, Niu CC, Chen LH, Fu TS, Wong CB. Surgical treatment of adjacent instability after lumbar spine fusion. Spine. 26:E519–E524. 2001.
Article8. Cho MJ, Chung CK, Kim CH. Screw loosening and migration after dynesys implantation. Korean J Spine. 9:300–303. 2012.
Article9. Choudhri TF, Mummaneni PV, Dhall SS, Eck JC, Groff MW, Ghogawala Z, et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 4: radiographic assessment of fusion status. J Neurosurg Spine. 21:23–30. 2014.
Article10. Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 303:1259–1265. 2010.
Article11. Eichholz KM, Ryken TC. Complications of revision spinal surgery. Neurosurg Focus. 15:E1. 2003.
Article12. Elowitz EH, Yanni DS, Chwajol M, Starke RM, Perin NI. Evaluation of indirect decompression of the lumbar spinal canal following minimally invasive lateral transpsoas interbody fusion: radiographic and outcome analysis. Minim Invasive Neurosurg. 54:201–206. 2011.
Article13. Fritsch EW, Heisel J, Rupp S. The failed back surgery syndrome: reasons, intraoperative findings, and long-term results: a report of 182 operative treatments. Spine. 21:626–633. 1996.14. Fujibayashi S, Hynes RA, Otsuki B, Kimura H, Takemoto M, Matsuda S. Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine (Phila Pa 1976). 40:E175–E182. 2015.
Article15. Jagersberg M, Schneider K, Schaller C, Richter M. ALIF versus TLIF for post-discectomy syndrome. J Neurol Surg A Cent Eur Neurosurg. 75:329–335. 2014.
Article16. Kim CH, Chung CK, Choi Y, Shin H, Woo JW, Kim SM, et al. The usefulness of a mobile device-based system for patient-reported outcomes in a spine outpatient clinic. Spine J. 16:843–850. 2016.
Article17. Kim CH, Chung CK, Hong HS, Kim EH, Kim MJ, Park BJ. Validation of a simple computerized tool for measuring spinal and pelvic parameters. J Neurosurg Spine. 16:154–162. 2012.
Article18. Kim CH, Chung CK, Park SB, Yang SH, Kim JH. A change in lumbar sagittal alignment after single-level anterior lumbar interbody fusion for lumbar degenerative spondylolisthesis with normal sagittal balance. Clin Spine Surg. 30:291–296. 2016.
Article19. Kim CH, Chung CK, Sohn S, Lee S, Park SB. Less invasive palliative surgery for spinal metastases. J Surg Oncol. 108:499–503. 2013.
Article20. Kim CH, Chung CK, Sohn S, Lee S, Park SB. The surgical outcome and the surgical strategy of percutaneous endoscopic discectomy for recurrent disk herniation. J Spinal Disord Tech. 27:415–422. 2014.
Article21. Kim DY, Lee SH, Lee HY, Lee HJ, Chang SB, Chung SK, et al. Validation of the korean version of the oswestry disability index. Spine (Phila Pa 1976). 30:E123–E127. 2005.
Article22. Leone A, Guglielmi G, Cassar-Pullicino VN, Bonomo L. Lumbar intervertebral instability: a review. Radiology. 245:62–77. 2007.
Article23. Marchi L, Abdala N, Oliveira L, Amaral R, Coutinho E, Pimenta L. Radiographic and clinical evaluation of cage subsidence after stand-alone lateral interbody fusion. J Neurosurg Spine. 19:110–118. 2013.
Article24. Nachemson A, Zdeblick TA, O’Brien JP. Lumbar disc disease with discogenic pain. What surgical treatment is most effective? Spine (Phila Pa 1976). 21:1835–1838. 1996.25. Nayak AN, Gutierrez S, Billys JB, Santoni BG, Castellvi AE. Biomechanics of lateral plate and pedicle screw constructs in lumbar spines instrumented at two levels with laterally placed interbody cages. Spine J. 13:1331–1338. 2013.
Article26. Palejwala SK, Sheen WA, Walter CM, Dunn JH, Baaj AA. Minimally invasive lateral transpsoas interbody fusion using a stand-alone construct for the treatment of adjacent segment disease of the lumbar spine: review of the literature and report of three cases. Clin Neurol Neurosurg. 124:90–96. 2014.
Article27. Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976). 29:1938–1944. 2004.
Article28. Park SJ, Lee CS, Chung SS, Kang SS, Park HJ, Kim SH. The ideal cage position for achieving both indirect neural decompression and segmental angle restoration in lateral lumbar interbody fusion (LLIF). Clin Spine Surg. 30:E784–E790. 2016.
Article29. Phan K, Thayaparan GK, Mobbs RJ. Anterior lumbar interbody fusion versus transforaminal lumbar interbody fusion--systematic review and meta-analysis. Br J Neurosurg. 29:705–711. 2015.
Article30. Rahm MD, Hall BB. Adjacent-segment degeneration after lumbar fusion with instrumentation: a retrospective study. J Spinal Disord. 9:392–400. 1996.31. Reis MT, Reyes PM, Bse , Altun I, Newcomb AG, Singh V, et al. Biomechanical evaluation of lateral lumbar interbody fusion with secondary augmentation. J Neurosurg Spine. 25:720–726. 2016.
Article32. Sears WR, Sergides IG, Kazemi N, Smith M, White GJ, Osburg B. Incidence and prevalence of surgery at segments adjacent to a previous posterior lumbar arthrodesis. Spine J. 11:11–20. 2011.
Article33. Song KS, Piyaskulkaew C, Chuntarapas T, Buchowski JM, Kim HJ, Park MS, et al. Dynamic radiographic criteria for detecting pseudarthrosis following anterior cervical arthrodesis. J Bone Joint Surg Am. 96:557–563. 2014.
Article34. Tempel ZJ, Gandhoke GS, Bolinger BD, Okonkwo DO, Kanter AS. Vertebral body fracture following stand-alone lateral lumbar interbody fusion (LLIF): report of two events out of 712 levels. Eur Spine J. 24(Suppl 3):409–413. 2015.
Article35. Terran J, Schwab F, Shaffrey CI, Smith JS, Devos P, Ames CP, et al. The SRS-Schwab adult spinal deformity classification: assessment and clinical correlations based on a prospective operative and nonoperative cohort. Neurosurgery. 73:559–568. 2013.36. Wang MY, Vasudevan R, Mindea SA. Minimally invasive lateral interbody fusion for the treatment of rostral adjacent-segment lumbar degenerative stenosis without supplemental pedicle screw fixation. J Neurosurg Spine. 21:861–866. 2014.
Article37. Watkins R 4th, Watkins R 3rd, Hanna R. Non-union rate with stand-alone lateral lumbar interbody fusion. Medicine (Baltimore). 93:e275. 2014.
Article38. Yee TJ, Terman SW, La Marca F, Park P. Comparison of adjacent segment disease after minimally invasive or open transforaminal lumbar interbody fusion. J Clin Neurosci. 21:1796–1801. 2014.
Article39. Zdeblick TA. A prospective, randomized study of lumbar fusion: Priliminary Results. Spine (Phila Pa 1976). 18:983–991. 1993.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Minimally Invasive Lateral Lumbar Interbody Fusion: Indications, Outcomes and Complications
- Comparison between Posterolateral Fusion with Pedicle Screw Fixation and Anterior Interbody Fusion with Pedicle Screw Fixation in Spondylolytic Spondylolisthesis of the Lumbar Spine
- Effect of the Pedicle Screw Fixation on the Anterior Lumbar Interbody Fusion Using the Freeze - Dried Structural Allograft
- Posterior Lumbar Intebody Fusion with Unilateral Transpedicular Screw and Contralateral Translaminar Facet Screw Fixation in Lumbar Spinal Stenosis
- The Comparison of Changes in the Dimensions of the Intervertebral Disc and Neural Foramen between Anterior Lumbar Interbody Fusion and Posterolateral Fusion in the Lumbar Spine