Korean J Neurotrauma.
2017 Oct;13(2):130-136. 10.13004/kjnt.2017.13.2.130.
The Efficacy of Fentanyl Transdermal Patch as the First-Line Medicine for the Conservative Treatment of Osteoporotic Compression Fracture
- Affiliations
-
- 1Department of Neurological Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 2Department of Emergency Medicine, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- 3Department of Neurological Surgery, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea. grandblue@gnah.co.kr
- KMID: 2394547
- DOI: http://doi.org/10.13004/kjnt.2017.13.2.130
Abstract
OBJECTIVE
There are no strong guidelines on how long or how we should undertake conservative treatment during the acute period of an osteoporotic vertebral compression fracture (VCF).
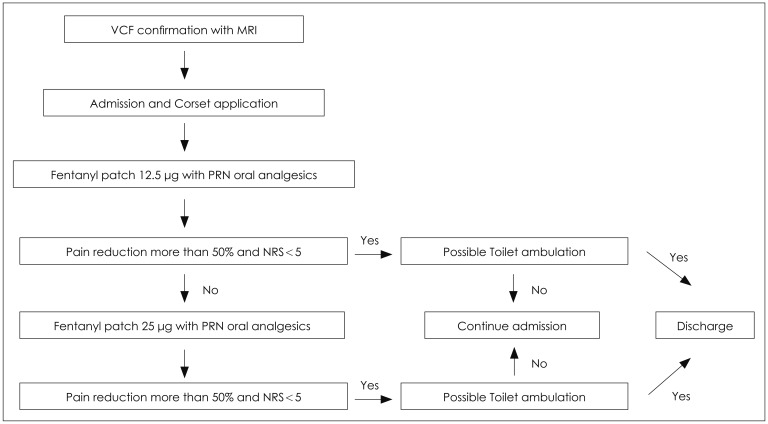
METHODS
We treated 202 patients with conservative treatment on VCF from March 2012 to August 2015. On inclusion criteria, 75 patients (22 males and 53 females) were included in the final analysis. After admission, a transdermal fentanyl patch with low dose (12.5 µg) application was attempted in all patients. In an unresponsive patient, the fentanyl patch was increased by 25 µg. After identifying the tolerable toilet ambulation of the patient without any assistance, hospital discharge was recommended. We classified two patient groups into one favorable group and one unfavorable group and compared several clinical and radiological factors.
RESULTS
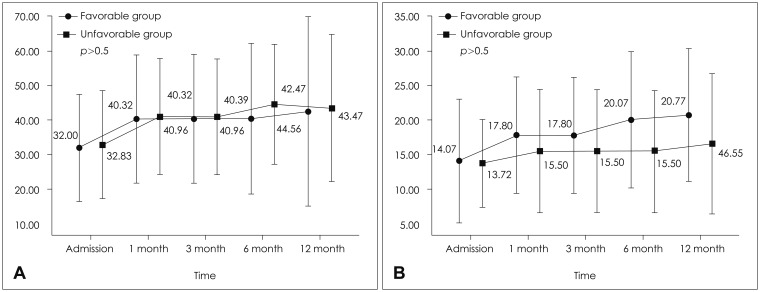
Among 75 patients, the clinical outcome of 57 patients (76%) was favorable, but that of 18 patients (24%) was unfavorable. In clinical outcomes, the numeric rating scale at 6 and 12 months and Odom's criteria at 12 months was significantly different between the favorable and the unfavorable groups. The dose of the patches used showed statistically significant differences between the two groups (p=0.001).
CONCLUSION
The only statistically significant affecting factor for an unfavorable outcome was the use of a higher dose fentanyl patch. Our data inferred that the unresponsiveness to a low-dose fentanyl patch could be helpful to select patients necessary for percutaneous vertebroplasty or kyphoplasty.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Percutaneous Vertebroplasty versus Conservative Treatment Using a Transdermal Fentanyl Patch for Osteoporotic Vertebral Compression Fractures
Younggyu Oh, Byungjou Lee, Subum Lee, Junghwan Kim, Jinhoon Park
J Korean Neurosurg Soc. 2019;62(5):594-602. doi: 10.3340/jkns.2019.0086.
Reference
-
1. Anderson PA, Froyshteter AB, Tontz WL Jr. Meta-analysis of vertebral augmentation compared with conservative treatment for osteoporotic spinal fractures. J Bone Miner Res. 2013; 28:372–382. PMID: 22991246.
Article2. Buchalter D, Kahanovitz N, Viola K, Dorsky S, Nordin M. Three-dimensional spinal motion measurements. Part 2: A noninvasive assessment of lumbar brace immobilization of the spine. J Spinal Disord. 1988; 1:284–286. PMID: 2980256.3. Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, et al. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. N Engl J Med. 2009; 361:557–568. PMID: 19657121.
Article4. Cha KH, Cho TG, Kim CH, Lee HK, Moon JG. Comparative study on the period of absolute bed rest of vertebral compression fracture. Korean J Spine. 2013; 10:144–148. PMID: 24757476.
Article5. Cherasse A, Muller G, Ornetti P, Piroth C, Tavernier C, Maillefert JF. Tolerability of opioids in patients with acute pain due to nonmalignant musculoskeletal disease. A hospital-based observational study. Joint Bone Spine. 2004; 71:572–576. PMID: 15589442.
Article6. Denaro V, Longo UG, Denaro L. Vertebroplasty versus conservative treatment for vertebral fractures. Lancet. 2010; 376:2071–2072. PMID: 21168046.
Article7. Esses SI, McGuire R, Jenkins J, Finkelstein J, Woodard E, Watters WC 3rd, et al. American academy of orthopaedic surgeons clinical practice guideline on: the treatment of osteoporotic spinal compression fractures. J Bone Joint Surg Am. 2011; 93:1934–1936. PMID: 22012531.8. Farrokhi MR, Alibai E, Maghami Z. Randomized controlled trial of percutaneous vertebroplasty versus optimal medical management for the relief of pain and disability in acute osteoporotic vertebral compression fractures. J Neurosurg Spine. 2011; 14:561–569. PMID: 21375382.
Article9. Grond S, Radbruch L, Lehmann KA. Clinical pharmacokinetics of transdermal opioids: focus on transdermal fentanyl. Clin Pharmacokinet. 2000; 38:59–89. PMID: 10668859.10. Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med. 2009; 361:569–579. PMID: 19657122.
Article11. Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine; current options and considerations for treatment. Spine J. 2006; 6:479–487. PMID: 16934715.
Article12. Klazen CA, Lohle PN, de Vries J, Jansen FH, Tielbeek AV, Blonk MC, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet. 2010; 376:1085–1092. PMID: 20701962.
Article13. Lantz SA, Schultz AB. Lumbar spine orthosis wearing. II. Effect on trunk muscle myoelectric activity. Spine (Phila Pa 1976). 1986; 11:838–842. PMID: 3810302.14. Li Y, Hai Y, Li L, Feng Y, Wang M, Cao G. Early effects of vertebroplasty or kyphoplasty versus conservative treatment of vertebral compression fractures in elderly polytrauma patients. Arch Orthop Trauma Surg. 2015; 135:1633–1636. PMID: 26559063.
Article15. Longo UG, Denaro V. Spinal augmentation: what have we learnt? Lancet. 2009; 373:1947. author reply 1947-1948. PMID: 19501742.
Article16. Longo UG, Loppini M, Denaro L, Maffulli N, Denaro V. Conservative management of patients with an osteoporotic vertebral fracture: a review of the literature. J Bone Joint Surg Br. 2012; 94:152–157. PMID: 22323677.17. Lukert BP. Vertebral compression fractures: how to manage pain, avoid disability. Geriatrics. 1994; 49:22–26.18. Lyles KW. Management of patients with vertebral compression fractures. Pharmacotherapy. 1999; 19:21s–24s. PMID: 9915558.
Article19. McGuire R. AAOS clinical practice guideline: the treatment of symptomatic osteoporotic spinal compression fractures. J Am Acad Orthop Surg. 2011; 19:183–184. PMID: 21368100.
Article20. Odom GL, Finney W, Woodhall B. Cervical disk lesions. J Am Med Assoc. 1958; 166:23–28. PMID: 13491305.
Article21. Park JH, Kim JH, Yun SC, Roh SW, Rhim SC, Kim CJ, et al. Evaluation of efficacy and safety of fentanyl transdermal patch (Durogesic D-TRANS) in chronic pain. Acta Neurochir (Wien). 2011; 153:181–190. PMID: 20821238.22. Pfeifer M, Begerow B, Minne HW. Effects of a new spinal orthosis on posture, trunk strength, and quality of life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil. 2004; 83:177–186. PMID: 15043351.23. Pfeifer M, Kohlwey L, Begerow B, Minne HW. Effects of two newly developed spinal orthoses on trunk muscle strength, posture, and quality-of-life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil. 2011; 90:805–815. PMID: 21681065.24. Pneumaticos SG, Triantafyllopoulos GK, Giannoudis PV. Advances made in the treatment of thoracolumbar fractures: current trends and future directions. Injury. 2013; 44:703–712. PMID: 23287553.
Article25. Prather H, Watson JO, Gilula LA. Nonoperative management of osteoporotic vertebral compression fractures. Injury. 2007; 38(Suppl 3):S40–S48. PMID: 17723791.
Article26. Rousing R, Andersen MO, Jespersen SM, Thomsen K, Lauritsen J. Percutaneous vertebroplasty compared to conservative treatment in patients with painful acute or subacute osteoporotic vertebral fractures: three-months follow-up in a clinical randomized study. Spine (Phila Pa 1976). 2009; 34:1349–1354. PMID: 19478654.27. Soultanis KC, Mavrogenis AF, Starantzis KA, Markopoulos C, Stavropoulos NA, Mimidis G, et al. When and how to operate on thoracic and lumbar spine fractures? Eur J Orthop Surg Traumatol. 2014; 24:443–451. PMID: 24158740.
Article28. Stevenson M, Gomersall T, Lloyd Jones M, Rawdin A, Hernandez M, Dias S, et al. Percutaneous vertebroplasty and percutaneous balloon kyphoplasty for the treatment of osteoporotic vertebral fractures: a systematic review and cost-effectiveness analysis. Health Technol Assess. 2014; 18:1–290.
Article29. Stillo JV, Stein AB, Ragnarsson KT. Low-back orthoses. Phys Med Rehabil Clin North Am. 1992; 2:57–94.
Article30. Voormolen MH, Mali WP, Lohle PN, Fransen H, Lampmann LE, van der Graaf Y, et al. Percutaneous vertebroplasty compared with optimal pain medication treatment: short-term clinical outcome of patients with subacute or chronic painful osteoporotic vertebral compression fractures. The VERTOS study. AJNR Am J Neuroradiol. 2007; 28:555–560. PMID: 17353335.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Vertebroplasty versus Conservative Treatment Using a Transdermal Fentanyl Patch for Osteoporotic Vertebral Compression Fractures
- The Effect of Fentanyl Patch in the Treatment of Intractable Postherpetic Neuralgia
- A Case of Fentanyl Toxicity with Misused Durogesic Transdermal Patch
- The Effectiveness of Transdermal Fentanyl Patch in Cancer Pain Patients
- Two Cases of Fentanyl Intoxication Through Overusing Fentanyl Patch