Korean J Neurotrauma.
2017 Oct;13(2):103-107. 10.13004/kjnt.2017.13.2.103.
Clinical Features of Interhemispheric Subdural Hematomas
- Affiliations
-
- 1Department of Neurosurgery, Soonchunhyang University Cheonan Hospital, Cheonan, Korea. ksleens@sch.ac.kr
- KMID: 2394542
- DOI: http://doi.org/10.13004/kjnt.2017.13.2.103
Abstract
OBJECTIVE
Interhemispheric subdural hematoma (IHSDH) is uncommon, because of their unusual location. However, it is a distinct lesion with its unique characteristics. We investigated clinical features and outcomes of consecutive 42 patients with IHSDH, retrospectively.
METHODS
From 2006 to 2015, we treated 105 patients with IHSDH. All patients were diagnosed by computed tomography (CT) or magnetic resonance imaging. We selected 42 patients with thick (3 mm or more) IHSDH. We retrospectively reviewed the clinical and radiological findings, management and outcomes.
RESULTS
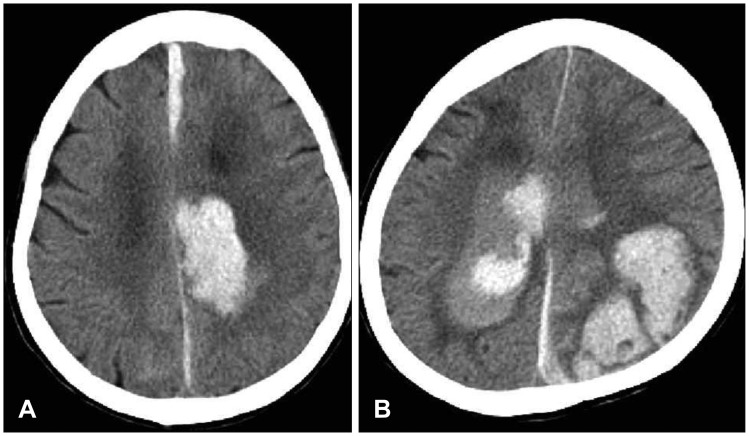
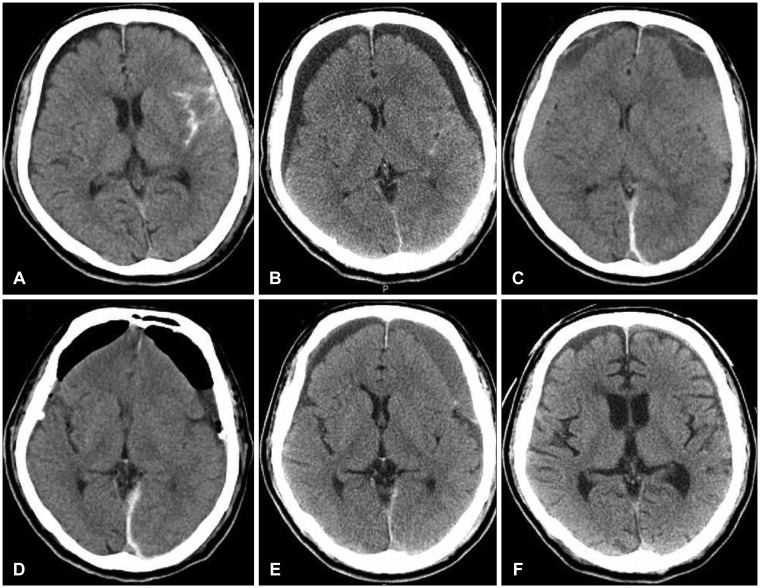
The male to female ratio was 2:1. Two thirds of the patients were over 60 years old. Slip or fall was the most common cause of trauma. The level of consciousness on admission was Glasgow Coma Scale (GCS) 13 to 15 in 25 patients. The most common symptom was headache. All IHSDH was hyperdense in CT at the time of diagnosis. IHSDH frequently accompanied convexity subdural hematoma. The outcome was favorable in 27 patients, however, six patients were expired. Twenty-two patients were managed conservatively. Surgery was performed in ten patients to remove the concurrent lesion. The outcome was poor in spontaneous one, patients with low GCS, and patients with conservative treatment.
CONCLUSION
IHSDH is rare especially the isolated one. The outcome was dependent to the severity of injury. Surgery may be helpful to remove the concurrent mass lesion, however, conservative treatment is generally preferred.
MeSH Terms
Figure
Reference
-
1. Alemdar M, Selekler HM, Efendi H. A non-traumatic interhemispheric subdural haematoma: presented with headache as the sole complaint. J Headache Pain. 2005; 6:48–50. PMID: 16362191.
Article2. Bartels RH, Verhagen WI, Prick MJ, Dalman JE. Interhemispheric subdural hematoma in adults: case reports and a review of the literature. Neurosurgery. 1995; 36:1210–1214. PMID: 7644007.3. Glista GG, Reichman OH, Brumlik J, Fine M. Interhemispheric subdural hematoma. Surg Neurol. 1978; 10:119–122. PMID: 705586.4. Lee KJ, Koh EJ, Choi HY. Interhemispheric chronic subdural hematoma showing falx syndrome: Case report. J Korean Neurosurg Soc. 2002; 32:268–271.5. Lee M, Kim MS, Yoon SW. Interhemispheric subdural hematoma presenting with falx syndrome after trauma. J Korean Neurotraumatol Soc. 2010; 6:158–161.
Article6. Psaltis A, Lath R, McDonald M. Acute interhemispheric subdural haematoma. J Clin Neurosci. 2004; 11:546–548. PMID: 15177409.
Article7. Rapana A, Lamaida E, Pizza V, Lepore P, Caputi F, Graziussi G. Inter-hemispheric scissure, a rare location for a traumatic subdural hematoma, case report and review of the literature. Clin Neurol Neurosurg. 1997; 99:124–129. PMID: 9213057.8. Requejo PR, Vaitsman RP, Paiva MS, Machado AL, Barroso MV, Salame JM, et al. Interhemispheric chronic subdural haematoma: case report and brief review of the literature. Brain Inj. 2010; 24:1039–1043. PMID: 20515363.
Article9. Sambasivan M. An overview of chronic subdural hematoma: experience with 2300 cases. Surg Neurol. 1997; 47:418–422. PMID: 9131021.
Article10. Shankar A, Joseph M, Chandy MJ. Interhemispheric subdural hematoma: an uncommon sequel of trauma. Neurol India. 2003; 51:63–64. PMID: 12865519.11. Shea YF, Li LF, Leung GKK, Chu LW. An uncommon complication of a fall in the elderly: Interhemispheric subdural hematoma. J Clin Gerontol Geriatr. 2013; 4:93–95.
Article12. Sogut O, Yigit M, Turkdogan KA, Yigit E, Gulen B, Sonmez E, et al. A distinct entity of subdural hematoma. J Clin Med Res. 2016; 8:178–179. PMID: 26767089.13. Takeda N, Kurihara E, Matsuoka H, Kose S, Tamaki N, Matsumoto S. Three cases of acute interhemispheric subdural hematoma. No Shinkei Geka. 1988; 16:87–92. PMID: 3283592.14. Takeuchi S, Takasato Y, Masaoka H, Hayakawa T, Yatsushige H, Sugawara T. Traumatic interhemispheric subdural haematoma: Study of 35 cases. J Clin Neurosci. 2010; 17:1527–1529. PMID: 20817537.
Article15. Wajima D, Yokota H, Ida Y, Nakase H. Spinal subdural hematoma associated with traumatic intracranial interhemispheric subdural hematoma. Neurol Med Chir (Tokyo). 2012; 52:636–639. PMID: 23006875.
Article16. Wang Y, Wang C, Cai S, Dong J, Yang L, Chen L, et al. Surgical management of traumatic interhemispheric subdural hematoma. Turk Neurosurg. 2014; 24:228–233. PMID: 24831365.17. Wu C, Liu Y, Yang C. Unusual cause of interhemispheric subdural hematoma: A case report. Neurosurg Q. 2015; 25:436–438.18. Yoo JS, Hu C, Hong SK, Kim HJ, Han YP. Clinical analysis of interhemispheric subdural hemorrhage and tentorial hemorrhage. J Korean Neurosurg Soc. 1991; 20:13–19.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Imterhemispheric Subdural Hematoma
- Computed tomography (CT) of the spontaneous resolution of traumatic epidural and subdural hematoma
- Traumatic Tentorial Hemorrhage
- Whole Lumbar Spinal Subdural Hematoma with Progressive Paraplegia after Lumbar Spinal Epidural Injection
- Interhemispheric Chronic Subdural Hematoma Showing Falx Syndrome: Case Report