Obstet Gynecol Sci.
2017 Sep;60(5):473-476. 10.5468/ogs.2017.60.5.473.
Genital tract cavernous hemangioma as a rare cause of postpartum hemorrhage
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Chonbuk National University Medical School, Jeonju, Korea. jh.lee@jbnu.ac.kr
- KMID: 2393848
- DOI: http://doi.org/10.5468/ogs.2017.60.5.473
Abstract
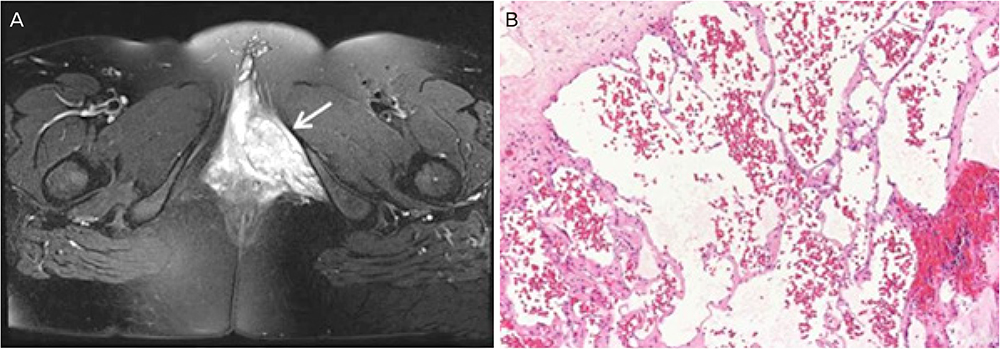
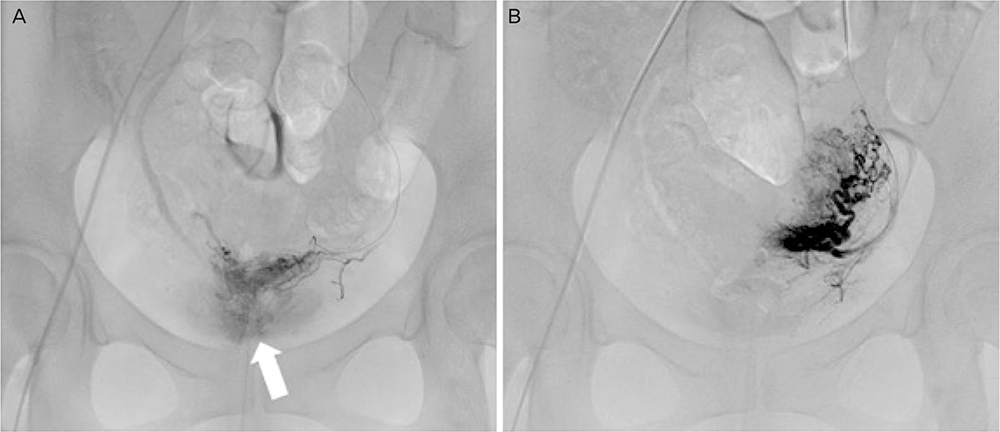
- Cavernous hemangiomas rarely involve the female genital tract. It is difficult to identify vascular malformations when these lesions are concealed in the vagina or deep vulva area. We present a rare case of vaginal cavernous hemangioma in a 30-year-old primiparous woman with an early severe postpartum hemorrhage (PPH) and delayed continuous bleeding from the episiotomy site. She was treated successfully with transarterial embolization of the left vaginal artery. To our knowledge, this is the first reported case of PPH caused by rupture of a vaginal hemangioma during vaginal delivery in English literature.
MeSH Terms
Figure
Reference
-
1. Kondi-Pafiti A, Kairi-Vassilatou E, Spanidou-Carvouni H, Kontogianni K, Dimopoulou K, Goula K. Vascular tumors of the female genital tract: a clinicopathological study of nine cases. Eur J Gynaecol Oncol. 2003; 24:48–50.2. Celik F, Arioz DT, Köken GN, Yilmazer M. Very rare cause of vaginal mass in pregnancy: cavernous hemangioma. J Obstet Gynaecol Res. 2012; 38:889–891.3. Gupta R, Singh S, Nigam S, Khurana N. Benign vascular tumors of female genital tract. Int J Gynecol Cancer. 2006; 16:1195–1200.4. Rezvani FF. Vaginal cavernous hemangioma in pregnancy. Obstet Gynecol. 1997; 89:824–825.5. Cebesoy FB, Kutlar I, Aydin A. A rare mass formation of the vulva: giant cavernous hemangioma. J Low Genit Tract Dis. 2008; 12:35–37.6. Wang S, Lang JH, Zhou HM. Venous malformations of the female lower genital tract. Eur J Obstet Gynecol Reprod Biol. 2009; 145:205–208.7. Saegusa T, Ito K, Oba N, Matsuda M, Kojima K, Tohyama K, et al. Enlargement of multiple cavernous hemangioma of the liver in association with pregnancy. Intern Med. 1995; 34:207–211.8. Chi JH, Manley GT, Chou D. Pregnancy-related vertebral hemangioma. Case report, review of the literature, and management algorithm. Neurosurg Focus. 2005; 19:E7.9. Conter RL, Longmire WP Jr. Recurrent hepatic hemangiomas. Possible association with estrogen therapy. Ann Surg. 1988; 207:115–119.10. Virk RK, Zhong J, Lu D. Diffuse cavernous hemangioma of the uterus in a pregnant woman: report of a rare case and review of literature. Arch Gynecol Obstet. 2009; 279:603–605.11. Taourel P, Dauzat M, Lafortune M, Pradel J, Rossi M, Bruel JM. Hemodynamic changes after transcatheter arterial embolization of hepatocellular carcinomas. Radiology. 1994; 191:189–192.12. Emoto M, Tamura R, Izumi H, Sukimoto S, Kawarabayashi T, Shirakawa K. Sonodynamic changes after transcatheter arterial embolization in a vaginal hemangioma: case report. Ultrasound Obstet Gynecol. 1997; 10:66–67.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Large Cavernous Hemangioma in the Jejunum of a 2-year-old Boy Treated by Laparoscopy-assisted Resection
- Cavernous Hemangioma of the Ovary
- Cavernous Hemangioma of the Renal Pelvis Associated with Renal Infarction and Hemorrhage: A Case Report
- Recurrent Cavernous Hemangioma of the Spermatic Cord
- A Case of Cavernous Hemangioma of the Cervix and Vagina