J Korean Ophthalmol Soc.
2017 Oct;58(10):1199-1204. 10.3341/jkos.2017.58.10.1199.
Bilateral Simple Ectopia Lentis Associated with FBN1 Gene Mutation
- Affiliations
-
- 1Department of Ophthalmology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. ckee@skku.edu
- 2Department of Laboratory Medicine and Genetics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2393174
- DOI: http://doi.org/10.3341/jkos.2017.58.10.1199
Abstract
- PURPOSE
To report a case of bilateral simple ectopia lentis associated with FBN1 gene mutation.
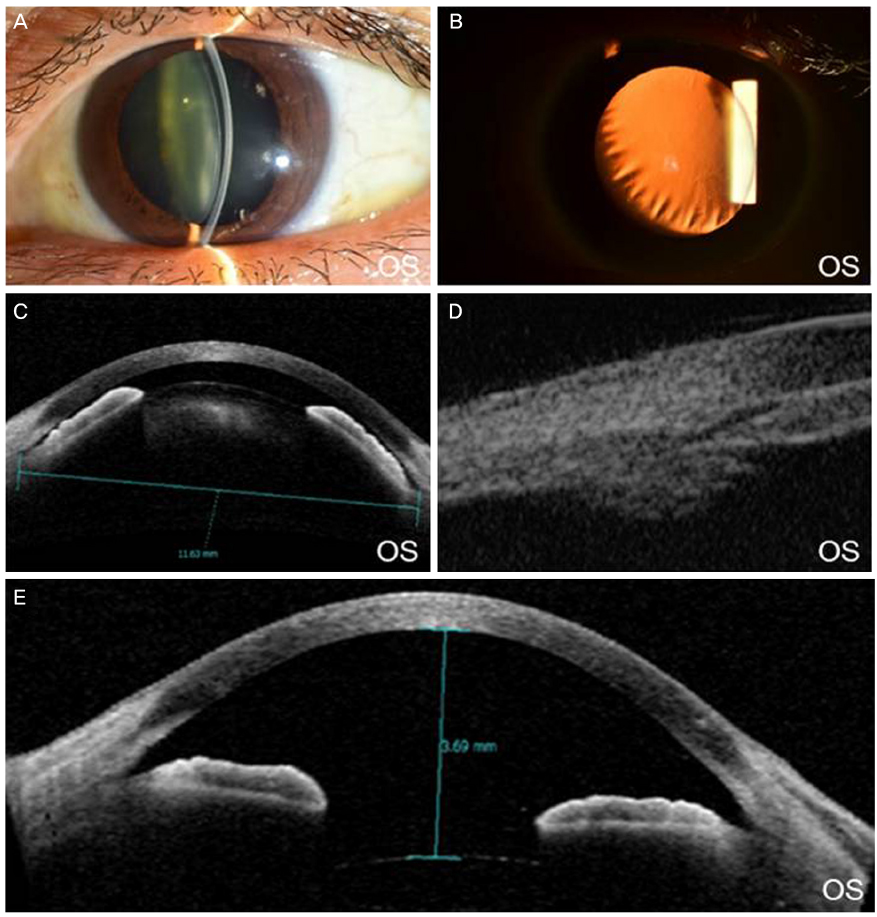
CASE SUMMARY
A 47-year-old women presented with a one-month history of ocular pain and decreased visual acuity of the right eye. She had a family history of crystalline lens dislocation but showed no systemic abnormality or trauma history. Intraocular pressure was 45 mmHg in the right eye, which showed a myopic shift (−6.5 D). The crystalline lens of the right eye was subluxated to the anterior chamber, and the angle was closed. Phacoemulsification with scleral fixation of the posterior chamber intraocular lens of the right eye was performed. After that, best corrected visual acuity of the right eye was 1.0, and intraocular pressure was 15 mmHg. After 2 years, she presented with intermittent ocular pain and decreased visual acuity of the left eye. The crystalline lens of the left eye was subluxated to the anterior chamber. Phacoemulsification with scleral fixation of the posterior chamber intraocular lens of the left eye was performed. After that, intermittent ocular pain and visual acuity of the left eye were improved. Genetic testing confirmed an FBN1 gene mutation in the patient.
CONCLUSIONS
A bilateral ectopia lentis patient without history of definite trauma should undergo complete systemic and ophthalmic examination to rule out accompanying disease, and a detailed family history should be collected. If hereditary ectopia lentis is suspected, genetic testing of probands and their family should be performed and will be helpful for genetic counseling and ophthalmic surveillance.
Keyword
MeSH Terms
Figure
Reference
-
1. Nelson LB, Maumenee IH. Ectopia lentis. Surv Ophthalmol. 1982; 27:143–160.2. Jarrett WH II. Dislocation of the lens. A study of 166 hospitalized cases. Arch Ophthalmol. 1967; 78:289–296.3. Neely DE, Plager DA. Management of ectopia lentis in children. Ophthalmol Clin North Am. 2001; 14:493–499.4. Sadiq MA, Vanderveen D. Genetics of ectopia lentis. Semin Ophthalmol. 2013; 28:313–320.5. Chandra A, Aragon-Martin JA, Hughes K, et al. A genotype-phenotype comparison of ADAMTSL4 and FBN1 in isolated ectopia lentis. Invest Ophthalmol Vis Sci. 2012; 53:4889–4896.6. Dureau P. Pathophysiology of zonular diseases. Curr Opin Ophthalmol. 2008; 19:27–30.7. Loeys BL, Dietz HC, Braverman AC, et al. The revised Ghent nosology for the Marfan syndrome. J Med Genet. 2010; 47:476–485.8. Mudd SH, Skovby F, Levy HL, et al. The natural history of homocystinuria due to cystathionine beta-synthase deficiency. Am J Hum Genet. 1985; 37:1–31.9. Shafique M, Muzaffar W, Ishaq M. The eye as a window to a rare disease: ectopia lentis and homocystinuria, a Pakistani perspective. Int Ophthalmol. 2016; 36:79–83.10. Yu YS, Awh JY, Lee JH. Management of ectopia lentis in children. J Korean Ophthalmol Soc. 1999; 40:1973–1978.11. Faivre L, Collod-Beroud G, Loeys BL, et al. Effect of mutation type and location on clinical outcome in 1,013 probands with Marfan syndrome or related phenotypes and FBN1 mutations: an international study. Am J Hum Genet. 2007; 81:454–466.12. Robinson PN, Godfrey M. The molecular genetics of Marfan syndrome and related microfibrillopathies. J Med Genet. 2000; 37:9–25.13. Deng T, Dong B, Zhang X, et al. Late-onset bilateral lens dislocation and glaucoma associated with a novel mutation in FBN1. Mol Vis. 2008; 14:1229–1233.14. Hubmacher D, Apte SS. ADAMTS proteins as modulators of microfibril formation and function. Matrix Biol. 2015; 47:34–43.15. Collin GB, Hubmacher D, Charette JR, et al. Disruption of murine Adamtsl4 results in zonular fiber detachment from the lens and in retinal pigment epithelium dedifferentiation. Hum Mol Genet. 2015; 24:6958–6974.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Three Cases of Simple Ectopia Lentis in One Family
- Identification of a Fibrillin-1 Gene Mutation in a Monozygotic Twin Presenting with Bilateral Juvenile-onset Ectopia Lentis
- Atypical Neonatal Marfan Syndrome with p.Glu1073Lys Mutation of FBN1: the First Case in Korea
- Management of Ectopia Lentis in Children
- Long Term Results of the Lensectomy in Children with Ectopia Lentis