J Korean Ophthalmol Soc.
2017 Oct;58(10):1122-1130. 10.3341/jkos.2017.58.10.1122.
Comparison of the Early Clinical Outcomes between Combined SMILE and Collagen Cross-linking versus SMILE
- Affiliations
-
- 1Onnuri Smile Eye Clinic, Seoul, Korea. ytchungc@daum.net
- KMID: 2393163
- DOI: http://doi.org/10.3341/jkos.2017.58.10.1122
Abstract
- PURPOSE
To compare the clinical outcome of combined small incision lenticule extraction and collagen cross-linking (SMILE Xtra) with SMILE.
METHODS
This study included 30 eyes from 15 patients who had undergone SMILE Xtra and a random sample of 30 eyes from 15 patients receiving SMILE alone during the same period. We obtained the following parameters from all patients: uncorrected (UDVA) and corrected distance visual acuity (CDVA), spherical equivalent (SE), efficacy and safety index, and corneal high-order aberrations.
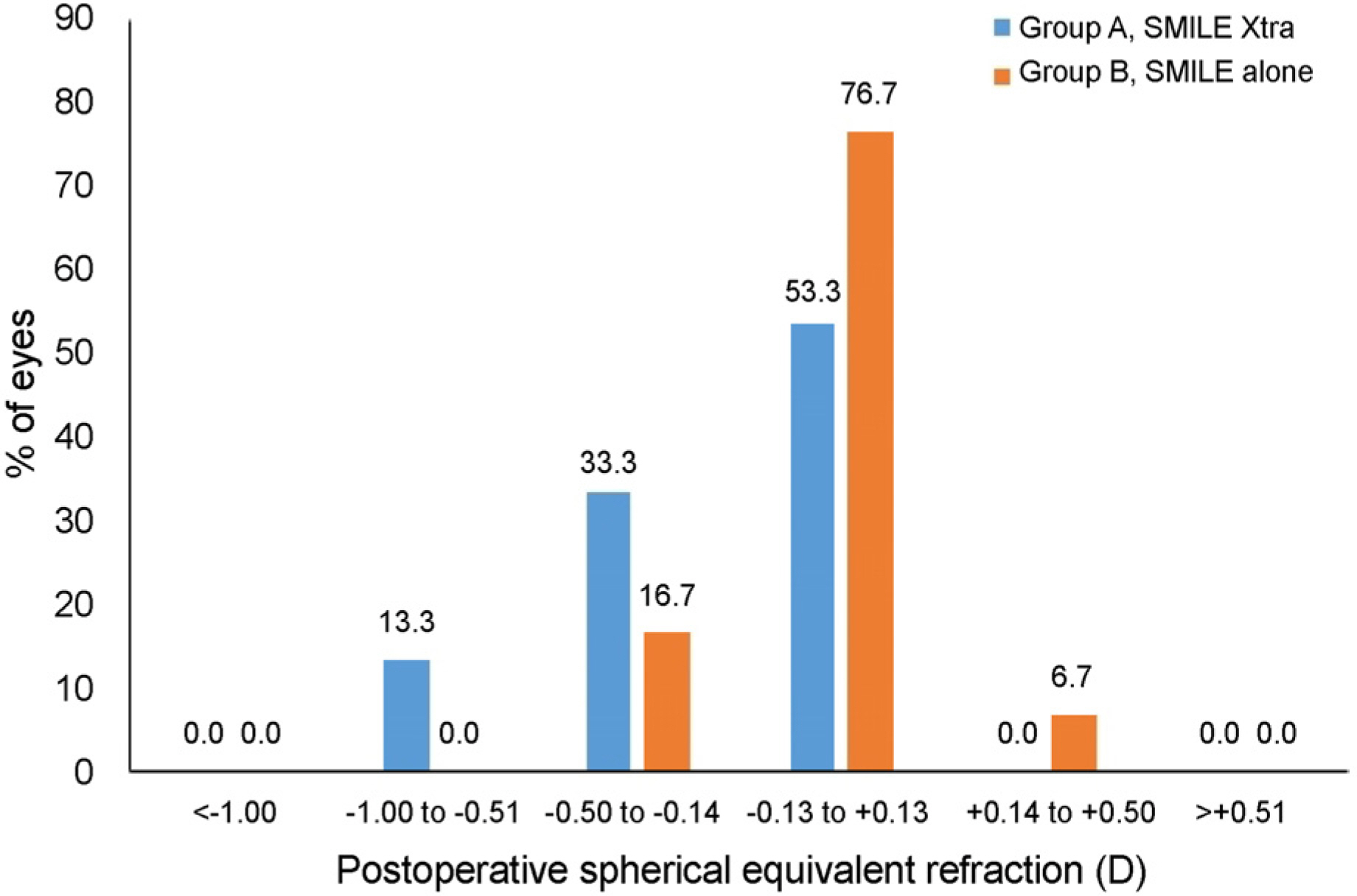
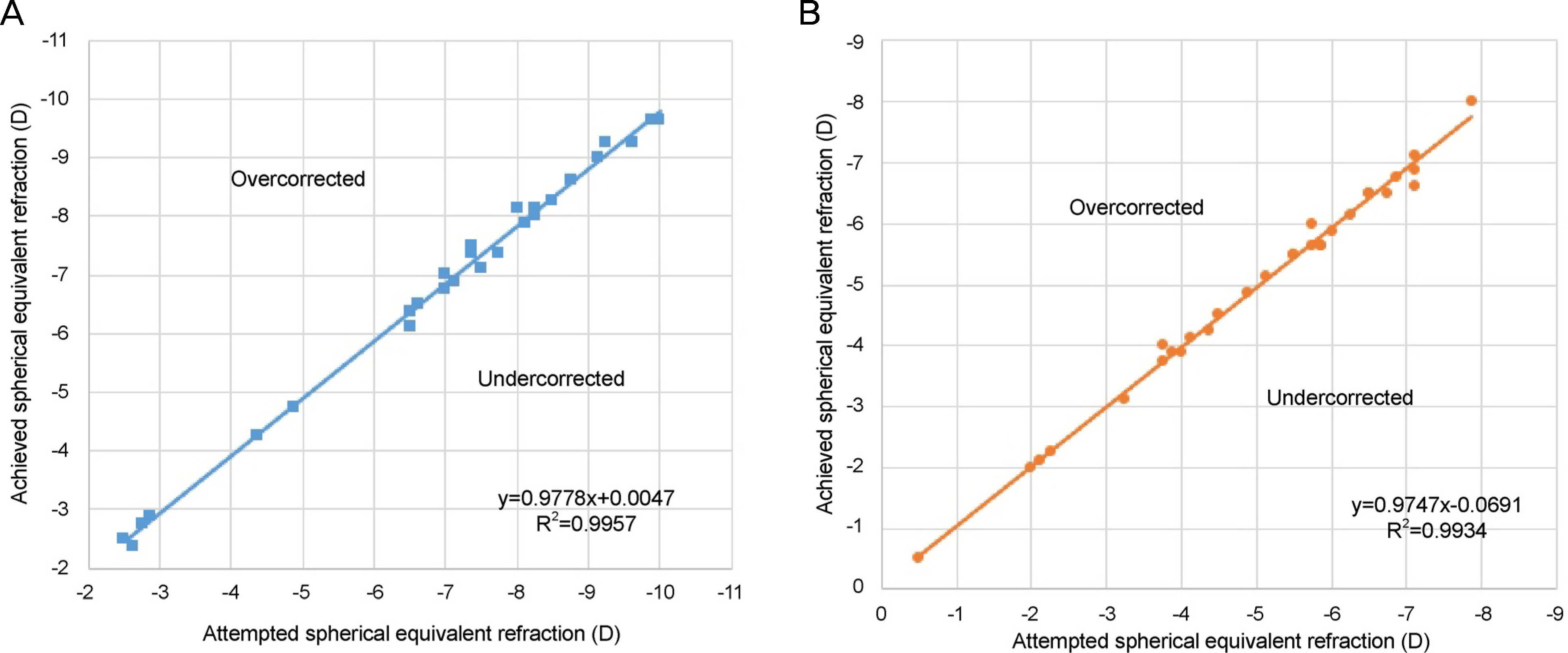
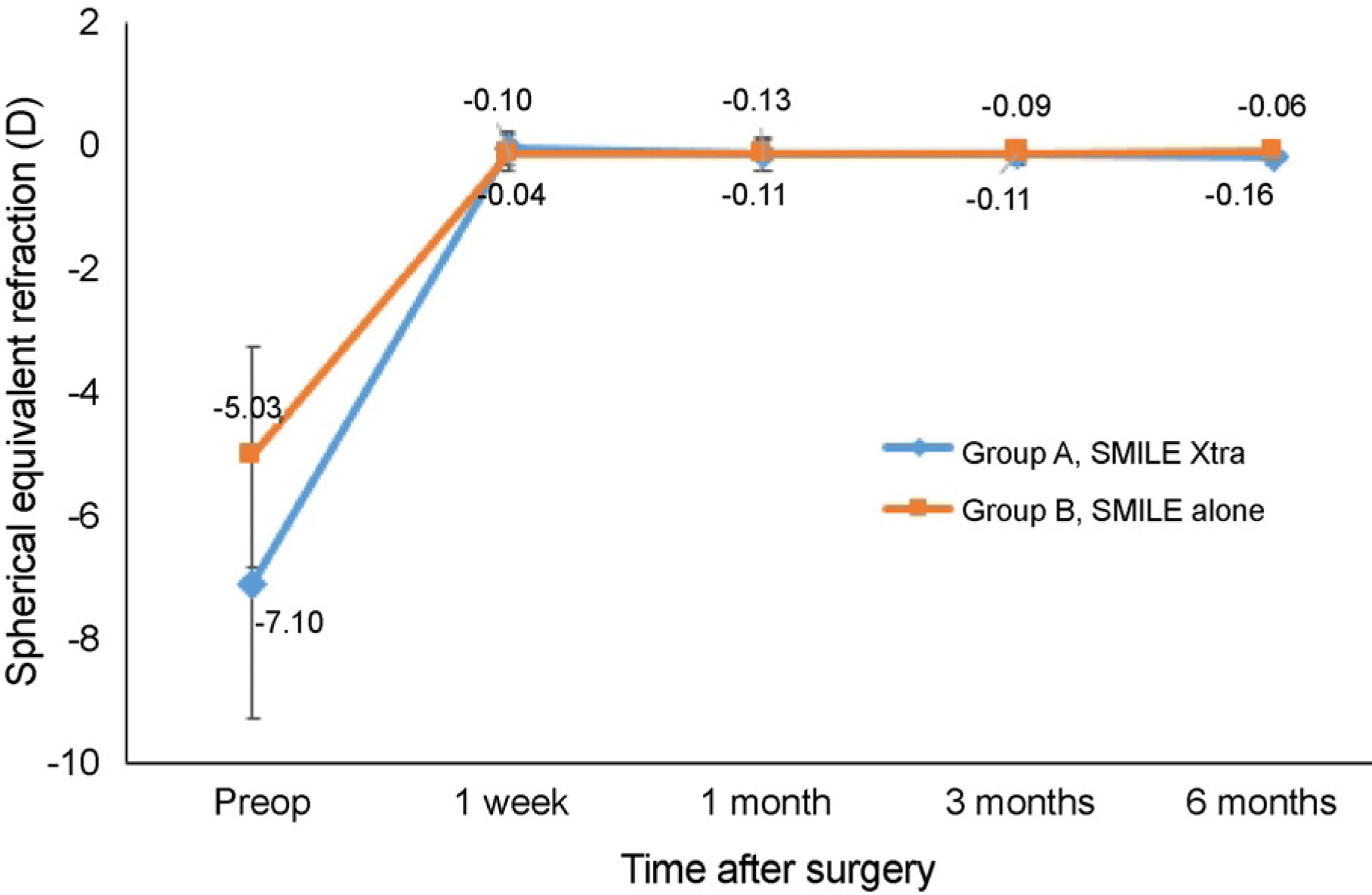
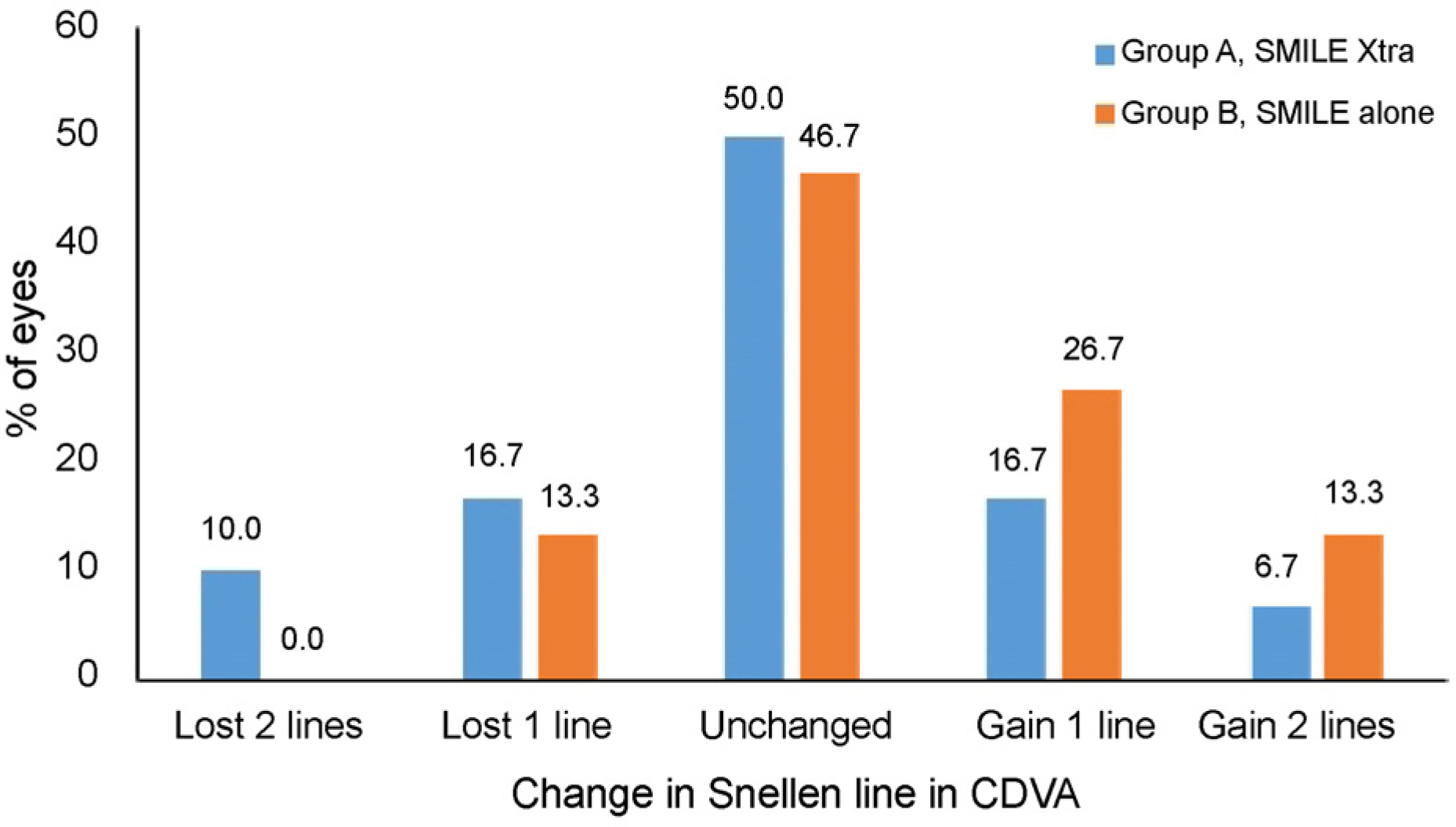
RESULTS
The SMILE Xtra group had higher preoperative SE and thinner central corneal and residual stromal bed thickness and optic zone diameter compared to the control group (p < 0.001). At 6 months, there was no significant difference in UDVA or CDVA between the two groups. The efficacy indices were 0.97 ± 0.16 and 1.05 ± 0.17 in the SMILE Xtra and control groups, respectively (p = 0.044), and there was no significant difference in safety index between the two groups during the follow-up period. Total corneal high-order aberrations numbered 2.59 ± 0.56 and 2.02 ± 0.41 in the SMILE Xtra and control groups, respectively (p < 0.001), and there was significant increase in spherical aberration and horizontal corneal aberration in both groups compared to preoperative results. Corneal haze was observed in 20% of eyes in the SMILE Xtra group, and no complication such as corneal ectasia was observed during the follow-up period.
CONCLUSIONS
SMILE Xtra had good early clinical outcome compared to SMILE alone. It appears that SMILE Xtra can be a good modality when the cornea is thin or SE is high. However, postoperative corneal haze should be considered.
Keyword
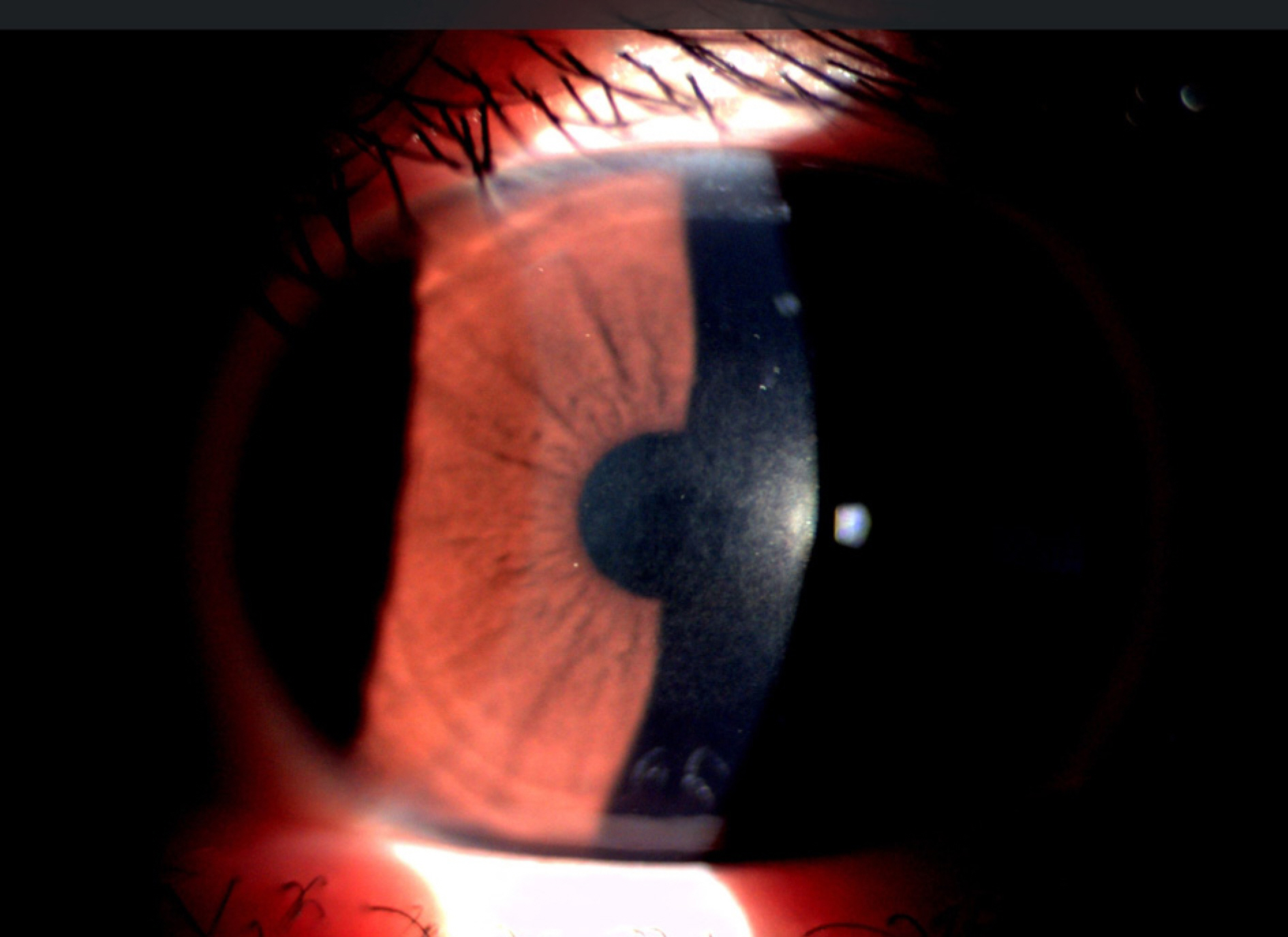
Figure
Reference
-
References
1. Binder PS. Ectasia after laser in situ keratomileusis. J Cataract Refract Surg. 2003; 29:2419–29.
Article2. Alió JL, Muftuoglu O, Ortiz D, et al. Ten-year follow-up of laser in situ keratomileusis for high myopia. Am J Ophthalmol. 2008; 145:55–64.
Article3. Raiskup-Wolf F, Hoyer A, Spoerl E, Pillunat LE. Collagen abdominal with riboflavin and ultraviolet-A light in keratoconus: long-term results. J Cataract Refract Surg. 2008; 34:796–801.4. Hafezi F, Kanellopoulos J, Wiltfang R, Seiler T. Corneal collagen crosslinking with riboflavin and ultraviolet A to treat induced abdominal after laser in situ keratomileusis. J Cataract Refract Surg. 2007; 33:2035–40.5. Kanellopoulos AJ, Binder PS. Collagen abdominal (CCL) with sequential topography-guided PRK: a temporizing alternative for keratoconus to penetrating keratoplasty. Cornea. 2007; 26:891–5.6. Kanellopoulos AJ, Pamel GJ. Review of current indications for combined very high fluence collagen abdominal and laser in situ keratomileusis surgery. Indian J Ophthalmol. 2013; 61:430–2.7. Shah R, Shah S, Sengupta S. Results of small incision lenticule abdominal: All-in-one femtosecond laser refractive surgery. J Cataract Refract Surg. 2011; 37:127–37.8. Wang Y, Cui C, Li Z, et al. Corneal ectasia 6.5 months after small-incision lenticule extraction. J Cataract Refract Surg. 2015; 41:1100–6.
Article9. Mattila JS, Holopainen JM. Bilateral ectasia after femtosecond abdominal-assisted small incision lenticule extraction (SMILE). J Refract Surg. 2016; 32:497–500.10. Ganesh S, Brar S. Clinical outcomes of small incision lenticule abdominal with accelerated abdominal (ReLEx SMILE Xtra) in abdominals with thin corneas and borderline topography. J Ophthalmol. 2015; 2015:263412.11. Randleman JB, Woodward M, Lynn MJ, Stulting RD. Risk abdominal for ectasia after corneal refractive surgery. Ophthalmology. 2008; 115:37–50.12. Nakamura K, Kurosaka D, Bissen-Miyajima H, Tsubota K. Intact corneal epithelium is essential for the prevention of stromal haze after laser assisted in situ keratomileusis. Br J Ophthalmol. 2001; 85:209–13.
Article13. Kobashi H, Kamiya K, Igarashi A, et al. Two-years results of small-incision lenticule extraction and wavefront-guided laser in situ keratomileusis for myopia. Acta Ophthalmol 2017 Jun 20. doi:. DOI: 10.1111/aos.13470. [Epub ahead of print].14. Cai WT, Liu QY, Ren CD, et al. Dry eye and corneal sensitivity abdominal small incision lenticule extraction and femtosecond laser-abdominal in situ keratomileusis: a Meta-analysis. Int J Ophthalmol. 2017; 10:632–8.
Article15. Jin Y, Wang Y, Xu L, et al. Comparison of the optical quality abdominal small incision lenticule extraction and femtosecond laser LASIK. J Ophthalmol. 2016; 2016:2507973.16. Wu D, Wang Y, Zhang L, et al. Corneal biomechanical effects: small-incision lenticule extraction versus femtosecond laser-abdominal laser in situ keratomileusis. J Cataract Refract Surg. 2014; 40:954–62.17. Wang D, Liu M, Chen Y, et al. Differences in the corneal abdominal changes after SMILE and LASIK. J Refract Surg. 2014; 30:702–7.18. Pedersen IB, Bak-Nielsen S, Vestergaard AH, et al. Corneal abdominal properties after LASIK, ReLEx flex, and ReLEx smile by Scheimpflug-based dynamic tonometry. Graefes Arch Clin Exp Ophthalmol. 2014; 252:1329–35.19. Sefat SM, Wiltfang R, Bechmann M, et al. Evaluation of changes in human corneas after femtosecond laser-assisted LASIK and small-incision lenticule extraction (SMILE) using non-contact abdominal and ultra-high-speed camera (Corvis ST). Curr Eye Res. 2016; 41:917–22.20. Sachdev G, Sachdev MS, Sachdev R, Gupta H. Unilateral corneal ectasia following small-incision lenticule extraction. J Cataract Refract Surg. 2015; 41:2014–8.
Article21. Tomita M, Yoshida Y, Yamamoto Y, et al. In vivo confocal laser abdominal of morphologic changes after simultaneous LASIK and accelerated collagen crosslinking for myopia: one-year results. J Cataract Refract Surg. 2014; 40:981–90.22. Kanellopoulos AJ, Asimellis G, Karabatsas C. Comparison of abdominal higher fluence corneal abdominal to control, in abdominal LASIK, one year results. Clin Ophthalmol. 2014; 8:2373–81.23. Ng AL, Chan TC, Cheng GP, et al. Comparison of the early clinical outcomes between combined small-incision lenticule extraction and collagen abdominal versus SMILE for myopia. J Ophthalmol. 2016; 2016:2672980.24. Wu W, Wang Y, Zhang H, et al. One-year visual outcome of small incision lenticule extraction (SMILE) surgery in high myopic eyes: retrospective cohort study. BMJ Open. 2016; 6:e010993.
Article25. Celik HU, Alagöz N, Yildirim Y, et al. Accelerated corneal abdominal concurrent with laser in situ keratomileusis. J Cataract Refract Surg. 2012; 38:1424–31.26. Kanellopoulos AJ, Asimellis G. Epithelial remodeling after abdominal laser-assisted high myopic LASIK: comparison of stand-alone with LASIK combined with prophylactic high-fluence abdominal. Cornea. 2014; 33:463–9.27. Alhayek A, Lu PR. Corneal collagen crosslinking in keratoconus and other eye disease. Int J Ophthalmol. 2015; 8:407–18.28. Greenstein SA, Fry KL, Bhatt J, Hersh PS. Natural history of abdominal haze after collagen crosslinking for keratoconus and corneal ectasia: Scheimpflug and biomicroscopic analysis. J Cataract Refract Surg. 2010; 36:2105–14.29. Koppen C, Vryghem JC, Gobin L, Tassignon MJ. Keratitis and abdominal scarring after UVA/riboflavin abdominal for keratoconus. J Refract Surg. 2009; 25:S819–23.
Article30. Kymionis GD, Tsoulnaras KI, Grentzelos MA, et al. Corneal abdominal demarcation line after standard and high-intensity collagen crosslinking determined with anterior segment optical coherence tomography. J Cataract Refract Surg. 2014; 40:736–40.31. Ağ ca A, Demirok A, Cankaya K, et al. Comparison of visual acuity and higher-order aberrations after femtosecond lenticule extraction and small-incision lenticule extraction. Cont Lens Anterior Eye. 2014; 37:292–6.32. Jin HY, Wan T, Wu F, Yao K. Comparison of visual results and higher-order aberrations after small incision lenticule extraction (SMILE): high myopia vs. mild to moderate myopia. BMC Ophthalmol. 2017; 17:118.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of the lip during smile in normal occlusion adults
- Treatment of Gingival Smile by Botulinum Toxin A
- Treatment of gummy smile using botulinum toxin: a review
- A Case of Suction Loss During SMILE and a Switch to LASIK
- Factors affecting smile esthetics in adults with different types of anterior overjet malocclusion