Korean J Gastroenterol.
2017 Oct;70(4):202-207. 10.4166/kjg.2017.70.4.202.
Intrahepatic Pancreatic Pseudocyst Complicated by Pancreatitis: A Case Report
- Affiliations
-
- 1Department of Surgery and Division of Gastroenterology, Chonnam National University Medical School, Gwangju, Korea. ckcho@jnu.ac.kr
- 2Department of Internal Medicine, Chonnam National University Medical School, Gwangju, Korea.
- KMID: 2392917
- DOI: http://doi.org/10.4166/kjg.2017.70.4.202
Abstract
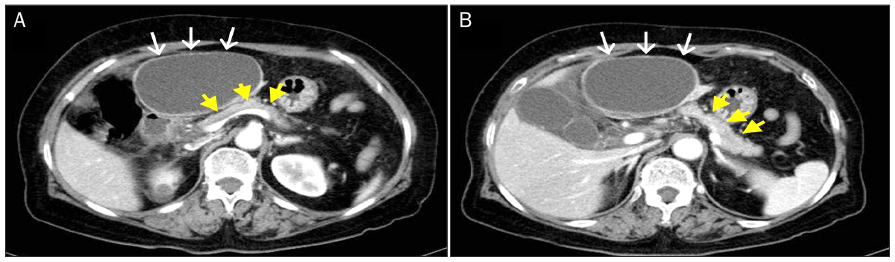
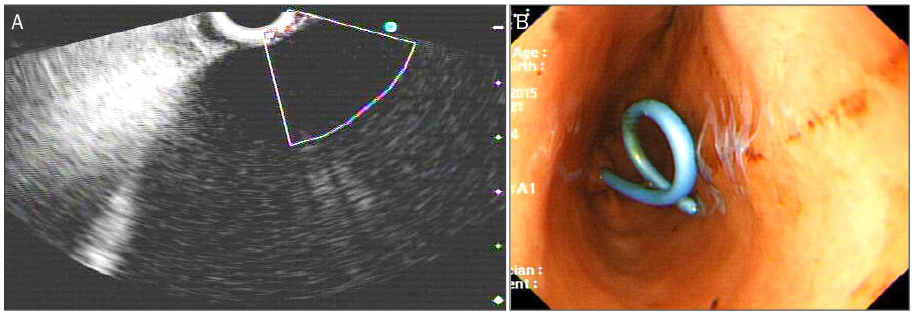
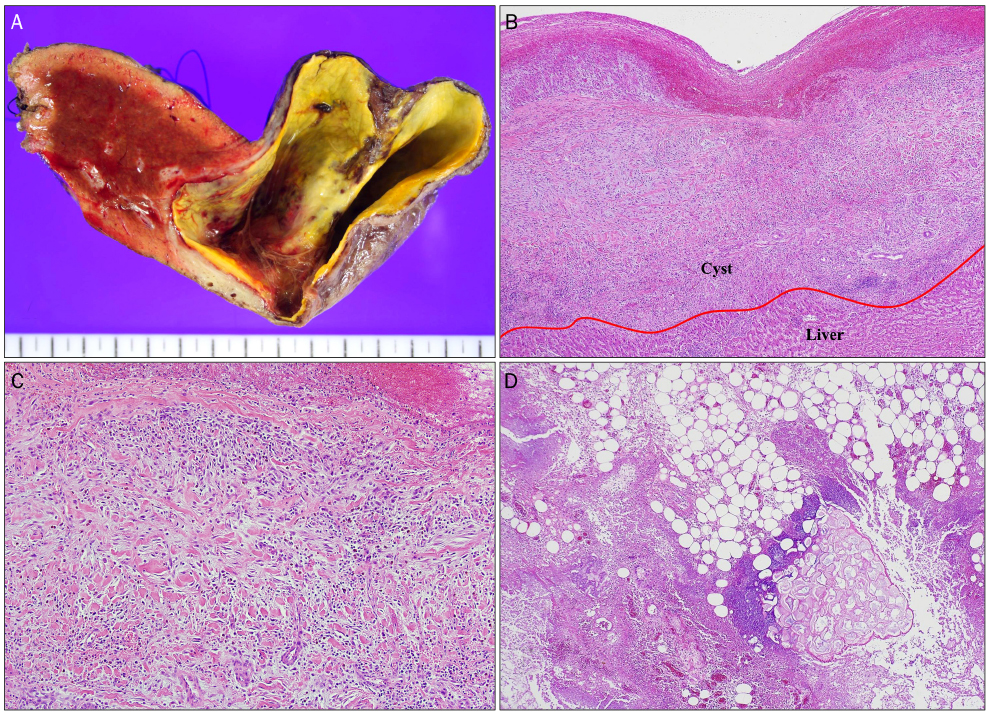
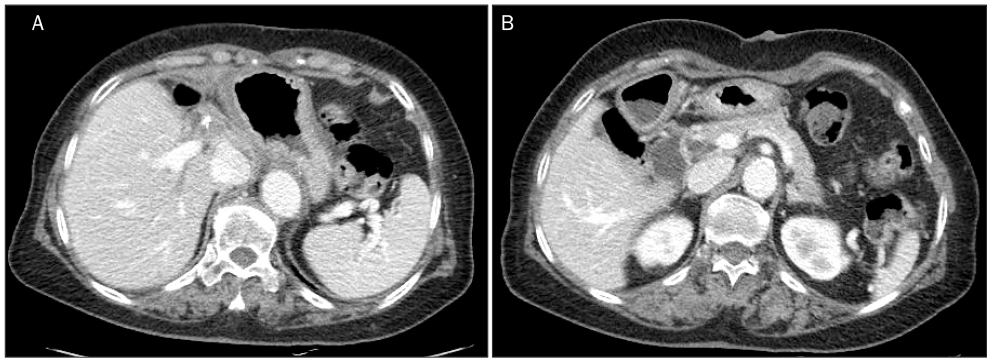
- Pancreatic pseudocyst is a common complication of acute pancreatitis. Pseudocysts are commonly observed in the lesser sac and retroperitoneum; they are rarely seen in the liver. Herein, we report a case of intrahepatic pseudocyst, complicated by asymptomatic groove pancreatitis, that has successfully been treated with hepatic resection. A 70-year-old woman was referred to our hospital with severe upper abdominal pain. Abdominal computed tomography scan showed 11×10 cm sized cystic lesion in the left lateral section of the liver. Appearance of the pancreas was relatively normal. Endoscopic aspiration revealed a high level of amylase in the cystic fluid. After endoscopy, signs of peritonitis were observed; then, a left hemihepatectomy was performed. Pathologic examination revealed an intrahepatic pancreatic pseudocyst. The presence of intrahepatic cystic lesion in patients with suspected pancreatitis should raise the suspicion of intrahepatic pseudocyst. Intrahepatic pancreatic pseudocysts may be the only clinical manifestation even without an episode of acute pancreatitis.
Keyword
MeSH Terms
Figure
Reference
-
1. Bardia A, Stoikes N, Wilkinson NW. Mediastinal pancreatic pseudocyst with acute airway obstruction. J Gastrointest Surg. 2006; 10:146–150.2. Skouras C, Skouras T, Pai M, Zacharakis E, Spalding D. Inguinoscrotal extension of a pancreatic collection: a rare complication of pancreatitis-case report and review of the literature. Updates Surg. 2013; 65:153–159.3. Demeusy A, Hosseini M, Sill AM, Cunningham SC. Intrahepatic pancreatic pseudocyst: a review of the world literature. World J Hepatol. 2016; 8:1576–1583.4. Bhasin DK, Rana SS, Chandail VS, et al. An intra-hepatic pancreatic pseudocyst successfully treated endoscopic transpapillary drainage alone. JOP. 2005; 6:593–597.5. Bhasin DK, Rana SS, Nanda M, et al. Endoscopic management of pancreatic pseudocysts at atypical locations. Surg Endosc. 2010; 24:1085–1091.6. Baydar B, Cantürk F, Alper E, et al. Intrahepatic localization of pancreatic pseudocyst: a case report. Turk J Gastroenterol. 2013; 24:447–449.7. Martínez-Sanz N, González-Valverde FM, Vicente-Ruiz M, Pastor-Pérez P, Ruiz-Marín M, Albarracín-Marín-Blázquez A. Intrahepatic pancreatic pseudocyst: a case report. Rev Esp Enferm Dig. 2015; 107:249–250.8. Yi CY, Na GJ, Baek HC, et al. A case of intrahepatic pseudocyst complicating acute pancreatitis. Korean J Gastroenterol. 2008; 51:56–59.9. Marrero JA, Ahn J, Rajender Reddy. ACG clinical guideline: the diagnosis and management of focal liver lesions. Am J Gastroenterol. 2014; 109:1328–1347.10. Casado D, Sabater L, Calvete J, et al. Multiple intrahepatic pseudocysts in acute pancreatitis. World J Gastroenterol. 2007; 13:4655–4657.11. Okuda K, Sugita S, Tsukada E, Sakuma Y, Ohkubo K. Pancreatic pseudocyst in the left hepatic lobe: a report of two cases. Hepatology. 1991; 13:359–363.12. Siegelman SS, Copeland BE, Saba GP, Cameron JL, Sanders RC, Zerhouni EA. CT of fluid collections associated with pancreatitis. AJR Am J Roentgenol. 1980; 134:1121–1132.13. Ancel D, Lefebvre M, Peyrin-Biroulet L, et al. Pancreatic pseudocysts of the right hepatic lobe during acute biliary pancreatitis. Gastroenterol Clin Biol. 2005; 29:743–745.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intrahepatic Bile Duct Dilatation Caused by Pancreatic Pseudocyst: A Case Report
- A Case of Intrahepatic Pseudocyst Complicating Acute Pancreatitis
- Pancreatic Pseudocyst-Portal Vein Fistula: Serial Imaging and Clinical Follow-up from Pseudocyst to Fistula
- Cardiac tamponade complicated by chronic recurrent pancreatitis
- A Case of Pancreatic Pseudocyst Presenting as Duodenal Bleeding