Korean Circ J.
2017 Jul;47(4):455-461. 10.4070/kcj.2016.0437.
Factors Influencing the Quality of Standardized Treatment for Patients with Post-Cardiac Arrest Syndrome
- Affiliations
-
- 1School of Public Health, Fudan University, Shanghai, China.
- 2Department of Intensive Care Unit, Traditional Chinese Medicine of Kunshan, Nanjing University of Chinese Medicine, Suzhou, China.
- 3Department of Emergency and Intensive Care Unit, Second Affiliated Hospital of Soochow University, Suzhou, China. lijunliusz@126.com
- KMID: 2392882
- DOI: http://doi.org/10.4070/kcj.2016.0437
Abstract
- BACKGROUND AND OBJECTIVES
For the present study, we investigated the factors that influence the quality of standardized treatment for patients with post-cardiac arrest syndrome (PCAS) to improve the quality of PCAS treatment.
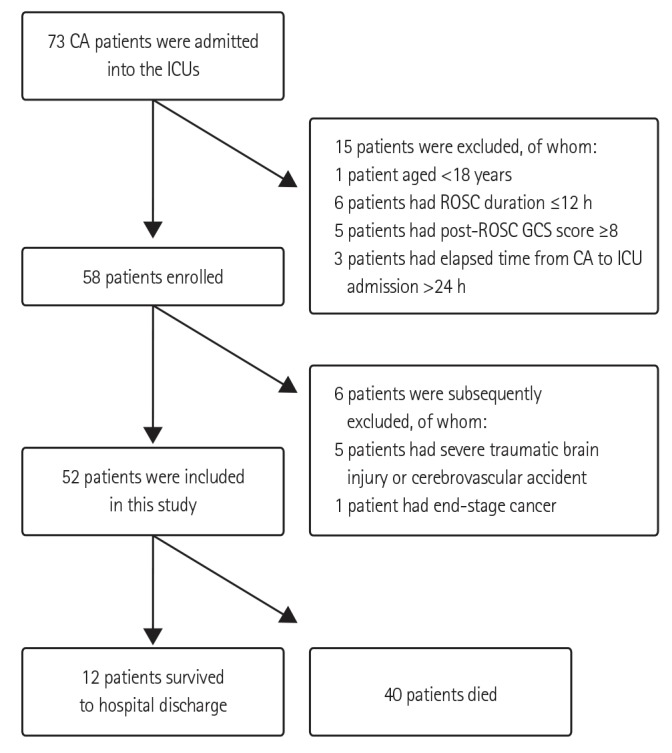
SUBJECTS AND METHODS
We collected data on patients with cardiac arrest (CA) who were admitted to the intensive care units (ICUs) of 11 hospitals-Class II Grade A or above-in Suzhou from January to October 2013. Indexes of standardized treatment were observed within 72 hrs of CA. We analyzed monitoring techniques, monitoring frequency, ICU human and material resources, and intensivists' knowledge of PCAS treatment to explore how those factors affected the management of patients with PCAS.
RESULTS
The bed/nurse ratio and the frequency with which core temperature was recorded correlated closely with the implementation of therapeutic hypothermia (TH) within 6 hrs of CA. The bed/doctor ratio and intensivists' knowledge about PCAS correlated closely with high-quality blood glucose control within 6 hrs of CA. Furthermore, the frequency with which core temperature was recorded was an independent factor influencing the quality of TH implementation, and the number times blood gas was analyzed was an independent factor influencing how well partial pressure of carbon dioxide was kept within the normal range in the 6 hrs after CA.
CONCLUSION
The frequency of core temperature measurements and the number of times blood gas is analyzed are the most important factors influencing the quality of standardized treatment for patients with PCAS.
MeSH Terms
Figure
Reference
-
1. Bernard SA, Gray TW, Buist MD, et al. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002; 346:557–563. PMID: 11856794.2. Oddo M, Schaller MD, Feihl F, Ribordy V, Liaudet L. From evidence to clinical practice: effective implementation of therapeutic hypothermia to improve patient outcome after cardiac arrest. Crit Care Med. 2006; 34:1865–1873. PMID: 16715035.3. Balan IS, Fiskum G, Hazelton J, Cotto-Cumba C, Rosenthal RE. Oximetry-guided reoxygenation improves neurological outcome after experimental cardiac arrest. Stroke. 2006; 37:3008–3013. PMID: 17068310.4. Peberdy MA, Callaway CW, Neumar RW, et al. Part 9: post-cardiac arrest care: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010; 122(18 Suppl 3):S768–S786. PMID: 20956225.5. Coles JP, Fryer TD, Coleman MR, et al. Hyperventilation following head injury: effect on ischemic burden and cerebral oxidative metabolism. Crit Care Med. 2007; 35:568–578. PMID: 17205016.6. Aufderheide TP. The problem with and benefit of ventilations: should our approach be the same in cardiac and respiratory arrest? Curr Opin Crit Care. 2006; 12:207–212. PMID: 16672778.7. Karanjia N, Geocadin RG. Post-cardiac arrest syndrome: update on brain injury management and prognostication. Curr Treat Options Neurol. 2011; 13:191–203. PMID: 21249482.8. Losert H, Sterz F, Roine RO, et al. Strict normoglycaemic blood glucose levels in the therapeutic management of patients within 12h after cardiac arrest might not be necessary. Resuscitation. 2008; 76:214–220. PMID: 17870226.9. Cueni-Villoz N, Devigili A, Delodder F, et al. Increased blood glucose variability during therapeutic hypothermia and outcome after cardiac arrest. Crit Care Med. 2011; 39:2225–2231. PMID: 21705888.10. Soar J, Nolan JP. Mild hypothermia for post cardiac arrest syndrome. BMJ. 2007; 335:459–460. PMID: 17823147.11. Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002; 346:549–556. PMID: 11856793.12. Abella BS, Rhee JW, Huang KN, Vanden Hoek TL, Becker LB. Induced hypothermia is underused after resuscitation from cardiac arrest: a current practice survey. Resuscitation. 2005; 64:181–186. PMID: 15680527.13. Tran BP, McGuire CV, Maloney MA. Use of mild therapeutic hypothermia improves outcomes in cardiac arrest. JAAPA. 2010; 23:43–48. PMID: 20232725.14. Liu L, Zhu J, Yang L, Zhang Y. Neurological outcomes of patients admitted to the intensive care unit for cardiac arrest. Chin Med J (Engl). 2014; 127:3024–3026. PMID: 25131245.15. Jena AB, Romley JA, Newton-Cheh C, Noseworthy P. Therapeutic hypothermia for cardiac arrest: real-world utilization trends and hospital mortality. J Hosp Med. 2012; 7:684–689. PMID: 23023977.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of Brain Injury after Post-cardiac Arrest Syndrome
- Management of post-cardiac arrest syndrome
- In-Hospital Cardiac Arrest: Patient Characteristics and Factors Influencing Survival and Neurologic Outcomes
- The Characteristics and the Predicting Factors of Hypoxic Myoclonus in the Post Cardiac Arrest Patient
- Cardiac Arrest During Pediatric Anesthesia