Korean J Pain.
2010 Mar;23(1):65-69.
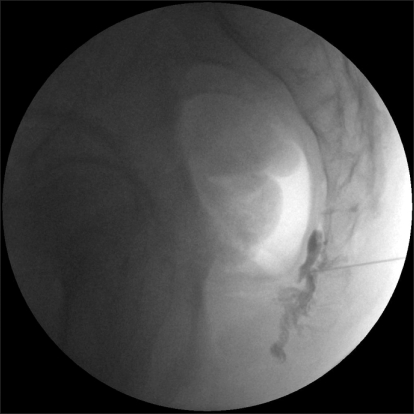
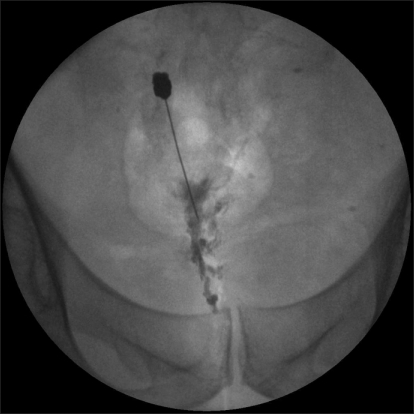
Ganglion Impar Block With Botulinum Toxin Type A for Chronic Perineal Pain -A Case Report-
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea. demoon@catholic.ac.kr
Abstract
- Chronic perineal pain is an often encountered problem, which produces a great degree of functional impairment and frustration to the patient and a challenge to the treating physician. The reason for this problem is that the region contains diverse anatomic structures with mixed somatic, visceral and autonomic innervations affecting bladder and bowel control and sexual function. A blockade of nociceptive and sympathetic supply to the perineal region, supplied through the ganglion impar has been shown to benefit patients with chronic perineal pain. Several options to this block have been described that chemical neurolysis, radiofrequency ablation etc. Although the analgesic effect of Botulinum toxin type A (BoNT-A) has long been considered secondary to its action for muscle relaxation, BoNT-A also affects the release of the neurotransmitters that are involved in pain perception. We describe a patient who was successfully given ganglion impar block with BoNT-A.
Keyword
MeSH Terms
Figure
Reference
-
1. Toshniwal GR, Dureja GP, Prashanth SM. Transsacrococcygeal approach to ganglion impar block for management of chronic perineal pain: a prospective observational study. Pain Physician. 2007; 10:661–666. PMID: 17876362.2. Lee HK, Yang SK, Lee HJ, Lee SY, Kim SM, Kim BS, et al. The effect of ganglion impar block for excessive perianal sweating. Korean J Pain. 1995; 8:363–366.3. Kim SK, Ahn CS, Cho YR, Lim SY, Shin KM, Hong SY, et al. Ganglion impar block in the management of rectal tenesmoid pain. Korean J Pain. 1996; 9:226–228.4. Reig E, Abejón D, del Pozo C, Insausti J, Contreras R. Thermocoagulation of the ganglion impar or ganglion of Walther: description of a modified approach. Preliminary results in chronic, nononcological pain. Pain Pract. 2005; 5:103–110. PMID: 17177756.
Article5. Mahant N, Clouston PD, Lorentz IT. The current use of botulinum toxin. J Clin Neurosci. 2000; 7:389–394. PMID: 10942658.
Article6. Welch MJ, Purkiss JR, Foster KA. Sensitivity of embryonic rat dorsal root ganglia neurons to Clostridium botulinum neurotoxins. Toxicon. 2000; 38:245–258. PMID: 10665805.
Article7. Aoki KR. Evidence for antinociceptive activity of botulinum toxin type A in pain management. Headache. 2003; 43(Suppl 1):S9–S15. PMID: 12887389.
Article8. Cui M, Khanijou S, Rubino J, Aoki KR. Subcutaneous administration of botulinum toxin A reduces formalin-induced pain. Pain. 2004; 107:125–133. PMID: 14715398.
Article9. Tait RC, Chibnall JT, Krause S. The pain disability index: psychometric properties. Pain. 1990; 40:171–182. PMID: 2308763.
Article10. Ailani J, Young WB. The role of nerve blocks and botulinum toxin injections in the management of cluster headaches. Curr Pain Headache Rep. 2009; 13:164–167. PMID: 19272284.
Article11. Carroll I, Clark JD, Mackey S. Sympathetic block with botulinum toxin to treat complex regional pain syndrome. Ann Neurol. 2009; 65:348–351. PMID: 19334078.
Article12. Jin L, Kollewe K, Krampfl K, Dengler R, Mohammadi B. Treatment of phantom limb pain with botulinum toxin type A. Pain Med. 2009; 10:300–303. PMID: 19207237.13. Park HJ, Lee Y, Lee J, Park C, Moon DE. The effects of botulinum toxin A on mechanical and cold allodynia in a rat model of neuropathic pain. Can J Anaesth. 2006; 53:470–477. PMID: 16636031.
Article14. Ranoux D, Attal N, Morain F, Bouhassira D. Botulinum toxin type A induces direct analgesic effects in chronic neuropathic pain. Ann Neurol. 2008; 64:274–283. PMID: 18546285.
Article15. Arezzo JC. Possible mechanisms for the effects of botulinum toxin on pain. Clin J Pain. 2002; 18(6 Suppl):S125–S132. PMID: 12569959.
Article16. Bach-Rojecky L, Lacković Z. Central origin of the antinociceptive action of botulinum toxin type A. Pharmacol Biochem Behav. 2009; 94:234–238. PMID: 19732788.
Article17. Mailis A, Furlan A. Sympathectomy for neuropathic pain. Cochrane Database Syst Rev. 2003; 2:CD002918. PMID: 12804444.18. Kim HJ, Seo K, Yum KW, Oh YS, Yoon TG, Yoon SM. Effects of botulinum toxin type A on the superior cervical ganglia in rabbits. Auton Neurosci. 2002; 102:8–12. PMID: 12492130.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Blockade of the Ganglion Impar for the Management of Intractable Coccygodynia
- Neurolytic Blockade of the Ganglion Impar for Relief of Cancer-Related Perianal Pain: A case report
- Treatment of Hyperhidrosis Occurring during Hemodialysis: Ganglion Impar Block: A case report
- The Effect of Ganglion Impar Block for Excessive Perianal Sweating: A case report
- The Effect of Ganglion Impar Block for Neoplastic Perineal Pain with Coccygeal Fracture