Allergy Asthma Respir Dis.
2017 Sep;5(5):298-301. 10.4168/aard.2017.5.5.298.
Acebrophylline-induced generalized fixed drug eruption confirmed by an oral provocation test
- Affiliations
-
- 1Department of Internal Medicine, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea. chansun@paik.ac.kr
- 2Department of Dermatology, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea.
- KMID: 2392407
- DOI: http://doi.org/10.4168/aard.2017.5.5.298
Abstract
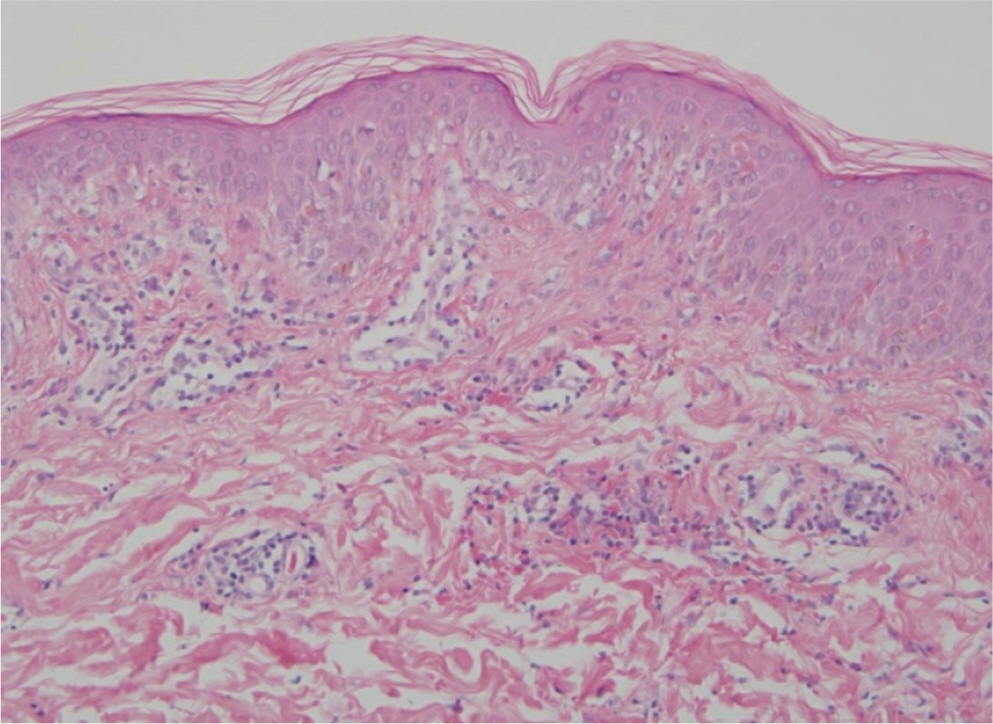
- The diagnosis of fixed drug eruption is straightforward because of characteristic findings, including recurrence of similar lesions at the same site and healing with residual hyperpigmentation. However, generalized or multiple fixed drug eruption, a rare variant form, can be a diagnostic challenge. Acebrophylline is a widely prescribed oral bronchodilator with mucosecretolyic and anti-inflammatory activity and is known to be relatively safe. A 34-year-old woman presented with recurrent numerous erythematous patches after ingestion of cold medications containing clarithromycin, loxoprofen, acebrophylline, and pseudoephedrine. Skin biopsy results showed vacuolar degeneration of the basal cell layer, scattered necrotic keratinocytes in the epidermis, and perivascular lymphohistiocytic infiltration in the upper dermis. A patch test showed negative results. However, in an oral challenge with acebrophylline 3 hours later, lesions reappeared at the same sites. To the best of our knowledge, this is the first case report of acebrophylline-induced generalized fixed drug eruption.
Keyword
MeSH Terms
Figure
Reference
-
1. Ozkaya E. Fixed drug eruption: state of the art. J Dtsch Dermatol Ges. 2008; 6:181–8.2. Goldrub N, Soares VR, Hamoui A, Zavattini G, Poli A. Therapeutic activity and tolerability profile of acebrophylline. Adv Ther. 1992; 9:107–15.3. Kuriachan S, Amberkar MB, Mohan MK, Shahul HA, Kishore MK. Ace-brophylline-induced angioedema. Indian J Pharmacol. 2015; 47:219–20.
Article4. Brocq L. Eruption erythémato-pigmentéefixé due à l'antipyrine. Ann Dermatol Syphiligr (Paris). 1894; 5:308–13.5. Lee AY. Fixed drug eruptions. Incidence, recognition, and avoidance. Am J Clin Dermatol. 2000; 1:277–85.6. Sawada Y, Nakamura M, Tokura Y. Generalized fixed drug eruption caused by pazufloxacin. Acta Derm Venereol. 2011; 91:600–1.
Article7. Can C, Akkelle E, Bay B, Arıcan O, Yalçın O, Yazicioglu M. Generalized fixed drug eruption in a child due to trimethoprim/sulfamethoxazole. Pediatr Allergy Immunol. 2014; 25:413–5.
Article8. Lipowicz S, Sekula P, Ingen-Housz-Oro S, Liss Y, Sassolas B, Dunant A, et al. Prognosis of generalized bullous fixed drug eruption: comparison with Stevens-Johnson syndrome and toxic epidermal necrolysis. Br J Dermatol. 2013; 168:726–32.
Article9. Shear NH, Knowles SR, Shapiro L. Cutaneous reactions to drugs. Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick's dermatology in general medicine. 7th ed.New York: McGraw-Hill;2007. p. 359–360.10. Jung JW, Cho SH, Kim KH, Min KU, Kang HR. Clinical features of fixed drug eruption at a tertiary hospital in Korea. Allergy Asthma Immunol Res. 2014; 6:415–20.
Article11. Heng YK, Yew YW, Lim DS, Lim YL. An update of fixed drug eruptions in Singapore. J Eur Acad Dermatol Venereol. 2015; 29:1539–44.
Article12. Mizukawa Y, Yamazaki Y, Shiohara T. In vivo dynamics of intraepidermal CD8+ T cells and CD4+ T cells during the evolution of fixed drug eruption. Br J Dermatol. 2008; 158:1230–8.13. Choi HJ, Ku JK, Kim MY, Kang H, Cho SH, Kim HO, et al. Possible role of Fas/Fas ligand-mediated apoptosis in the pathogenesis of fixed drug eruption. Br J Dermatol. 2006; 154:419–25.
Article14. Cho YT, Lin JW, Chen YC, Chang CY, Hsiao CH, Chung WH, et al. Generalized bullous fixed drug eruption is distinct from Stevens-Johnson syndrome/toxic epidermal necrolysis by immunohistopathological features. J Am Acad Dermatol. 2014; 70:539–48.
Article15. Dharamsi FM, Michener MD, Dharamsi JW. Bullous fixed drug eruption masquerading as recurrent Stevens Johnson syndrome. J Emerg Med. 2015; 48:551–4.
Article16. Elm MK, Murchland MR. Multifocal, fixed-drug eruption masquerading as recurrent erythema multiforme. J Drugs Dermatol. 2012; 11:244–6.17. Sowden JM, Smith AG. Multifocal fixed drug eruption mimicking erythema multiforme. Clin Exp Dermatol. 1990; 15:387–8.
Article18. Inserra DW, Camisa C. Erythema multiforme-like fixed drug eruption. Cutis. 1989; 44:223–5.19. Yoo SH, Kang SJ, Lee AY. Nonpigmenting fixed drug eruption to etodol-ac. Korean J Dermatol. 1999; 37:673–5.20. Shiohara T. Fixed drug eruption: pathogenesis and diagnostic tests. Curr Opin Allergy Clin Immunol. 2009; 9:316–21.
Article