Ann Surg Treat Res.
2017 Oct;93(4):195-202. 10.4174/astr.2017.93.4.195.
Novel anal sphincter saving procedure with partial excision of levator-ani muscle in rectal cancer invading ipsilateral pelvic floor
- Affiliations
-
- 1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. namkyuk@yuhs.ac
- KMID: 2392369
- DOI: http://doi.org/10.4174/astr.2017.93.4.195
Abstract
- PURPOSE
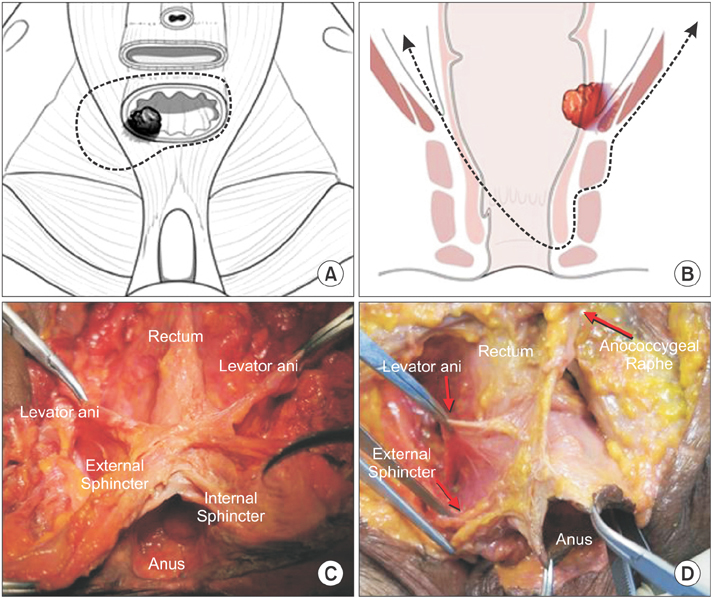
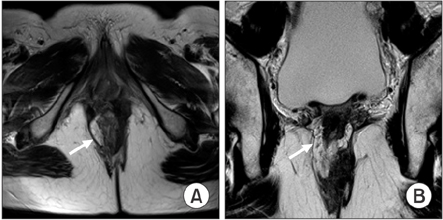
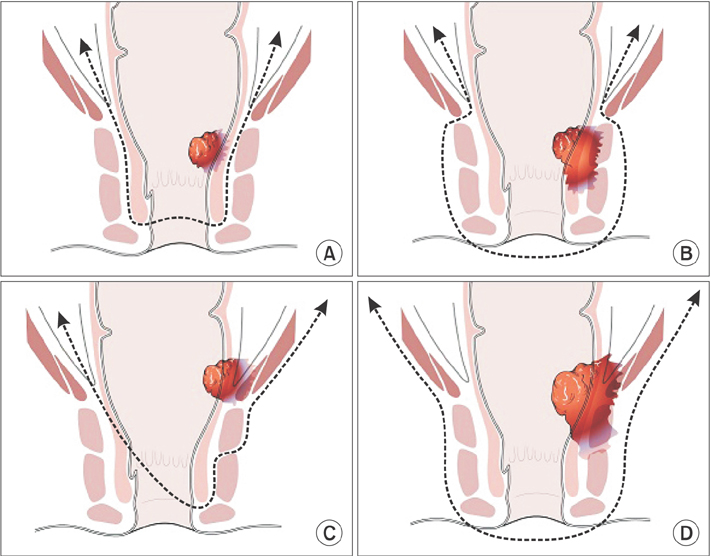
Tumors at the level of the anorectal junction had required total levator-ani muscle excision to achieve an adequate resection margin. However, in the cases of tumor invading ipsilateral levator-ani muscle and intact external sphincter, en bloc resection of rectum with levator-ani muscle including tumor would be possible. This hemilevator excision (HLE) technique enables preserving the anal sphincter function while obtaining oncologic clearance and avoiding permanent colostomy in those patients. This study aimed to evaluate the surgical outcomes and feasibility of HLE.
METHODS
Data on 13 consecutive patients who underwent HLE for pathologically proven low rectal cancer were retrospectively collected. All 13 patients presented low rectal cancer at the anorectal ring level that was suspected to invade or abut to the ipsilateral side of the levator-ani muscle.
RESULTS
A secure resection margin was achieved in all cases, and anastomotic leakage occurred in 2 patients. During follow-up, 3 patients experienced tumor recurrence (2 systemic and 1 local). Among 6 patients who underwent diverting ileostomy closure after the index operation, 2 complained of fecal incontinence. The other 4 patients without fecal incontinence showed <10 times of bowel movement per day. Accessing their incontinence scale, mean Wexner score was 9.4.
CONCLUSION
HLE is a novel sphincter-preserving technique that can be a treatment option for low rectal cancer invading ipsilateral levator-ani muscle, which has been an indication for abdominoperineal resection (APR) or extralevator APR. However, the long-term oncologic and functional outcomes of this procedure still need to be assessed to confirm its validity.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Critical and Challenging Issues in the Surgical Management of Low-Lying Rectal Cancer
Aeris Jane D. Nacion, Youn Young Park, Seung Yoon Yang, Nam Kyu Kim
Yonsei Med J. 2018;59(6):703-716. doi: 10.3349/ymj.2018.59.6.703.
Reference
-
1. Marr R, Birbeck K, Garvican J, Macklin CP, Tiffin NJ, Parsons WJ, et al. The modern abdominoperineal excision: the next challenge after total mesorectal excision. Ann Surg. 2005; 242:74–82.2. Heald RJ, Smedh RK, Kald A, Sexton R, Moran BJ. Abdominoperineal excision of the rectum--an endangered operation. Norman Nigro Lectureship. Dis Colon Rectum. 1997; 40:747–751.3. Nagtegaal ID, van de, Marijnen CA, van Krieken JH, Quirke P, et al. Dutch Colorectal Cancer Group. Low rectal cancer: a call for a change of approach in abdominoperineal resection. J Clin Oncol. 2005; 23:9257–9264.4. Holm T, Ljung A, Häggmark T, Jurell G, Lagergren J. Extended abdominoperineal resection with gluteus maximus flap reconstruction of the pelvic floor for rectal cancer. Br J Surg. 2007; 94:232–238.5. West NP, Finan PJ, Anderin C, Lindholm J, Holm T, Quirke P. Evidence of the oncologic superiority of cylindrical abdominoperineal excision for low rectal cancer. J Clin Oncol. 2008; 26:3517–3522.6. West NP, Anderin C, Smith KJ, Holm T, Quirke P. European Extralevator Abdominoperineal Excision Study Group. Multicentre experience with extralevator abdominoperineal excision for low rectal cancer. Br J Surg. 2010; 97:588–599.7. Williams NS, Dixon MF, Johnston D. Reappraisal of the 5 centimetre rule of distal excision for carcinoma of the rectum: a study of distal intramural spread and of patients’ survival. Br J Surg. 1983; 70:150–154.8. Schiessel R, Karner-Hanusch J, Herbst F, Teleky B, Wunderlich M. Intersphincteric resection for low rectal tumours. Br J Surg. 1994; 81:1376–1378.9. Camilleri-Brennan J, Steele RJ. Quality of life after treatment for rectal cancer. Br J Surg. 1998; 85:1036–1043.10. Fucini C, Elbetti C, Messerini L. Anatomic plane of separation between external anal sphincter and puborectalis muscle: clinical implications. Dis Colon Rectum. 1999; 42:374–379.11. Fucini C, Elbetti C, Petrolo A, Casella D. Excision of the levator muscles with external sphincter preservation in the treatment of selected low T4 rectal cancers. Dis Colon Rectum. 2002; 45:1697–1705.12. Jorge JM, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Rectum. 1993; 36:77–97.13. Watanabe M, Teramoto T, Hasegawa H, Kitajima M. Laparoscopic ultralow anterior resection combined with per anum intersphincteric rectal dissection for lower rectal cancer. Dis Colon Rectum. 2000; 43:10 Suppl. S94–S97.14. Mandard AM, Dalibard F, Mandard JC, Marnay J, Henry-Amar M, Petiot JF, et al. Pathologic assessment of tumor regression after preoperative chemoradiotherapy of esophageal carcinoma. Clinicopathologic correlations. Cancer. 1994; 73:2680–2686.15. Zhou X, Sun T, Xie H, Zhang Y, Zeng H, Fu W. Extralevator abdominoperineal excision for low rectal cancer: a systematic review and meta-analysis of the short-term outcome. Colorectal Dis. 2015; 17:474–481.16. De Nardi P, Summo V, Vignali A, Capretti G. Standard versus extralevator abdominoperineal low rectal cancer excision outcomes: a systematic review and metaanalysis. Ann Surg Oncol. 2015; 22:2997–3006.17. Akasu T, Takawa M, Yamamoto S, Ishiguro S, Yamaguchi T, Fujita S, et al. Intersphincteric resection for very low rectal adenocarcinoma: univariate and multivariate analyses of risk factors for recurrence. Ann Surg Oncol. 2008; 15:2668–2676.18. Cong JC, Chen CS, Ma MX, Xia ZX, Liu DS, Zhang FY. Laparoscopic intersphincteric resection for low rectal cancer: comparison of stapled and manual coloanal anastomosis. Colorectal Dis. 2014; 16:353–358.19. Kang J, Hur H, Min BS, Lee KY, Kim NK. Robotic coloanal anastomosis with or without intersphincteric resection for low rectal cancer: starting with the perianal approach followed by robotic procedure. Ann Surg Oncol. 2012; 19:154–155.20. Weiser MR, Quah HM, Shia J, Guillem JG, Paty PB, Temple LK, et al. Sphincter preservation in low rectal cancer is facilitated by preoperative chemoradiation and intersphincteric dissection. Ann Surg. 2009; 249:236–242.21. Rullier E, Sa Cunha A, Couderc P, Rullier A, Gontier R, Saric J. Laparoscopic intersphincteric resection with coloplasty and coloanal anastomosis for mid and low rectal cancer. Br J Surg. 2003; 90:445–451.22. Bretagnol F, Rullier E, Couderc P, Rullier A, Saric J. Technical and oncological feasibility of laparoscopic total mesorectal excision with pouch coloanal anastomosis for rectal cancer. Colorectal Dis. 2003; 5:451–453.23. Leong QM, Son DN, Cho JS, Baek SJ, Kwak JM, Amar AH, et al. Robot-assisted intersphincteric resection for low rectal cancer: technique and short-term outcome for 29 consecutive patients. Surg Endosc. 2011; 25:2987–2992.24. Park JS, Kim NK, Kim SH, Lee KY, Lee KY, Shin JY, et al. Multicentre study of robotic intersphincteric resection for low rectal cancer. Br J Surg. 2015; 102:1567–1573.25. Martin ST, Heneghan HM, Winter DC. Systematic review of outcomes after intersphincteric resection for low rectal cancer. Br J Surg. 2012; 99:603–612.26. Laurent C, Paumet T, Leblanc F, Denost Q, Rullier E. Intersphincteric resection for low rectal cancer: laparoscopic vs open surgery approach. Colorectal Dis. 2012; 14:35–41.27. Hamada M, Matsumura T, Matsumoto T, Teraishi F, Ozaki K, Nakamura T, et al. Video. Advantages of the laparoscopic approach for intersphincteric resection. Surg Endosc. 2011; 25:1661–1663.28. Lee SH, Lim S, Kim JH, Lee KY. Robotic versus conventional laparoscopic surgery for rectal cancer: systematic review and meta-analysis. Ann Surg Treat Res. 2015; 89:190–201.29. Baek SJ, Al-Asari S, Jeong DH, Hur H, Min BS, Baik SH, et al. Robotic versus laparoscopic coloanal anastomosis with or without intersphincteric resection for rectal cancer. Surg Endosc. 2013; 27:4157–4163.30. Bretagnol F, Rullier E, Laurent C, Zerbib F, Gontier R, Saric J. Comparison of functional results and quality of life between intersphincteric resection and conventional coloanal anastomosis for low rectal cancer. Dis Colon Rectum. 2004; 47:832–838.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Robotic Partial Excision of Levator-Ani Muscle for Locally Advanced Low Rectal Cancer Invading Ipsilateral Pelvic Floor
- Levator Ani Muscle Posterior Midline Incision Method for Diffrentiation of Anal Fistulas Involving Ischioretal and Pelvirectal Spaces
- Female Longitudinal Anal Muscles or Conjoint Longitudinal Coats Extend into the Subcutaneous Tissue along the Vaginal Vestibule: A Histological Study Using Human Fetuses
- Selective Approach to Sphincter-Saving Procedure after Chemoradiation in Low Rectal Cancer
- Sharp Pelvic Dissection for Abdominoperineal Resection for Distal Rectal Cancer Based on Anatomical and MRI Knowledge