Clin Exp Vaccine Res.
2013 Jan;2(1):34-39.
Current status of vaccine development for tularemia preparedness
- Affiliations
-
- 1Division of High-Risk Pathogen Research, Center for Infectious Diseases, Korea National Institute of Health, Cheongwon, Korea.
- 2Division of Zoonoses, Center for Immunology and Pathology, Korea National Institute of Health, Cheongwon, Korea. kyuhwang@nih.go.kr
Abstract
- Tularemia is a high-risk infectious disease caused by Gram-negative bacterium Francisella tularensis. Due to its high fatality at very low colony-forming units (less than 10), F. tularensis is considered as a powerful potential bioterrorism agent. Vaccine could be the most efficient way to prevent the citizen from infection of F. tularensis when the bioterrorism happens, but officially approved vaccine with both efficacy and safety is not developed yet. Research for the development of tularemia vaccine has been focusing on the live attenuated vaccine strain (LVS) for long history, still there are no LVS confirmed for the safety which should be an essential factor for general vaccination program. Furthermore the LVS did not show protection efficacy against high-risk subspecies tularensis (type A) as high as the level against subspecies holarctica (type B) in human. Though the subunit or recombinant vaccine candidates have been considered for better safety, any results did not show better prevention efficacy than the LVS candidate against F. tularensis infection. Currently there are some more trials to develop vaccine using mutant strains or nonpathogenic F. novicida strain, but it did not reveal effective candidates overwhelming the LVS either. Difference in the protection efficacy of LVS against type A strain in human and the low level protection of many subunit or recombinant vaccine candidates lead the scientists to consider the live vaccine development using type A strain could be ultimate answer for the tularemia vaccine development.
MeSH Terms
Figure
Reference
-
1. Pechous RD, McCarthy TR, Zahrt TC. Working toward the future: insights into Francisella tularensis pathogenesis and vaccine development. Microbiol Mol Biol Rev. 2009. 73:684–711.
Article2. Saslaw S, Eigelsbach HT, Prior JA, Wilson HE, Carhart S. Tularemia vaccine study. II. Respiratory challenge. Arch Intern Med. 1961. 107:702–714.3. Saslaw S, Eigelsbach HT, Wilson HE, Prior JA, Carhart S. Tularemia vaccine study. I. Intracutaneous challenge. Arch Intern Med. 1961. 107:689–701.4. Dennis DT, Inglesby TV, Henderson DA, et al. Tularemia as a biological weapon: medical and public health management. JAMA. 2001. 285:2763–2773.5. Keim P, Johansson A, Wagner DM. Molecular epidemiology, evolution, and ecology of Francisella. Ann N Y Acad Sci. 2007. 1105:30–66.
Article6. Pullen RL, Stuart BM. Tularemia: analysis of 225 cases. JAMA. 1945. 129:495–500.7. Evans ME, Gregory DW, Schaffner W, McGee ZA. Tularemia: a 30-year experience with 88 cases. Medicine (Baltimore). 1985. 64:251–269.8. Conlan JW, KuoLee R, Shen H, Webb A. Different host defences are required to protect mice from primary systemic vs pulmonary infection with the facultative intracellular bacterial pathogen, Francisella tularensis LVS. Microb Pathog. 2002. 32:127–134.
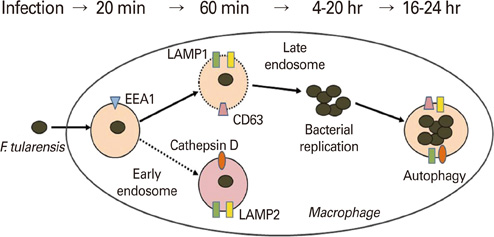
Article9. Hopla CE. The multiplication of tularemia organisms in the lone star tick. Am J Hyg. 1955. 61:371–380.10. Checroun C, Wehrly TD, Fischer ER, Hayes SF, Celli J. Autophagy-mediated reentry of Francisella tularensis into the endocytic compartment after cytoplasmic replication. Proc Natl Acad Sci U S A. 2006. 103:14578–14583.
Article11. Clemens DL, Lee BY, Horwitz MA. Virulent and avirulent strains of Francisella tularensis prevent acidification and maturation of their phagosomes and escape into the cytoplasm in human macrophages. Infect Immun. 2004. 72:3204–3217.
Article12. Francis E. Tularemia. JAMA. 1925. 84:1243–1250.
Article13. World Health Organization. WHO/CDS/EPR/2007.7. WHO guidelines on tularaemia. 2007. Geneva: World Health Organization.14. Kaufmann AF, Meltzer MI, Schmid GP. The economic impact of a bioterrorist attack: are prevention and postattack intervention programs justifiable? Emerg Infect Dis. 1997. 3:83–94.
Article15. Tigertt WD. Soviet viable Pasteurella tularensis vaccines: a review of selected articles. Bacteriol Rev. 1962. 26:354–373.
Article16. Christopher GW, Cieslak TJ, Pavlin JA, Eitzen EM Jr. Biological warfare: a historical perspective. JAMA. 1997. 278:412–417.
Article17. Foshay L, Hesselbrock WH, Wittenberg HJ, Rodenberg AH. Vaccine prophylaxis against tularemia in man. Am J Public Health Nations Health. 1942. 32:1131–1145.
Article18. Centers for Disease Control and Prevention. Summary of notifiable diseases, United States, 1997. MMWR Morb Mortal Wkly Rep. 1998. 46:ii–vii. 3–87.19. Gray CG, Cowley SC, Cheung KK, Nano FE. The identification of five genetic loci of Francisella novicida associated with intracellular growth. FEMS Microbiol Lett. 2002. 215:53–56.
Article20. Nano FE, Zhang N, Cowley SC, et al. A Francisella tularensis pathogenicity island required for intramacrophage growth. J Bacteriol. 2004. 186:6430–6436.
Article21. Shen H, Chen W, Conlan JW. Mice sublethally infected with Francisella novicida U112 develop only marginal protective immunity against systemic or aerosol challenge with virulent type A or B strains of F. tularensis. Microb Pathog. 2004. 37:107–110.
Article22. Wu TH, Hutt JA, Garrison KA, Berliba LS, Zhou Y, Lyons CR. Intranasal vaccination induces protective immunity against intranasal infection with virulent Francisella tularensis biovar A. Infect Immun. 2005. 73:2644–2654.
Article23. Hall JD, Woolard MD, Gunn BM, et al. Infected-host-cell repertoire and cellular response in the lung following inhalation of Francisella tularensis Schu S4, LVS, or U112. Infect Immun. 2008. 76:5843–5852.
Article24. Golovliov I, Ericsson M, Akerblom L, Sandstrom G, Tarnvik A, Sjostedt A. Adjuvanticity of ISCOMs incorporating a T cell-reactive lipoprotein of the facultative intracellular pathogen Francisella tularensis. Vaccine. 1995. 13:261–267.
Article25. Thomas RM, Titball RW, Oyston PC, et al. The immunologically distinct O antigens from Francisella tularensis subspecies tularensis and Francisella novicida are both virulence determinants and protective antigens. Infect Immun. 2007. 75:371–378.
Article26. Bakshi CS, Malik M, Mahawar M, et al. An improved vaccine for prevention of respiratory tularemia caused by Francisella tularensis SchuS4 strain. Vaccine. 2008. 26:5276–5288.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Adenovirus Vectors: Excellent Tools for Vaccine Development
- Animal models for dengue vaccine development and testing
- The first pediatric case of tularemia in Korea: manifested with pneumonia and possible infective endocarditis
- The Strategic Plans for Preparedness and Response to Bioterrorism
- COVID-19 vaccines development in Africa: a review of current situation and existing challenges of vaccine production