Infect Chemother.
2017 Sep;49(3):230-235. 10.3947/ic.2017.49.3.230.
Campylobacter jejuni Bacteremia in a Liver Cirrhosis Patient and Review of Literature: A Case Study
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea. heejinmd@korea.ac.kr
- 2Asia Pacific Influenza Institute, Korea University College of Medicine, Seoul, Korea.
- 3Department of Laboratory Medicine, Korea University College of Medicine, Seoul, Korea.
- KMID: 2391431
- DOI: http://doi.org/10.3947/ic.2017.49.3.230
Abstract
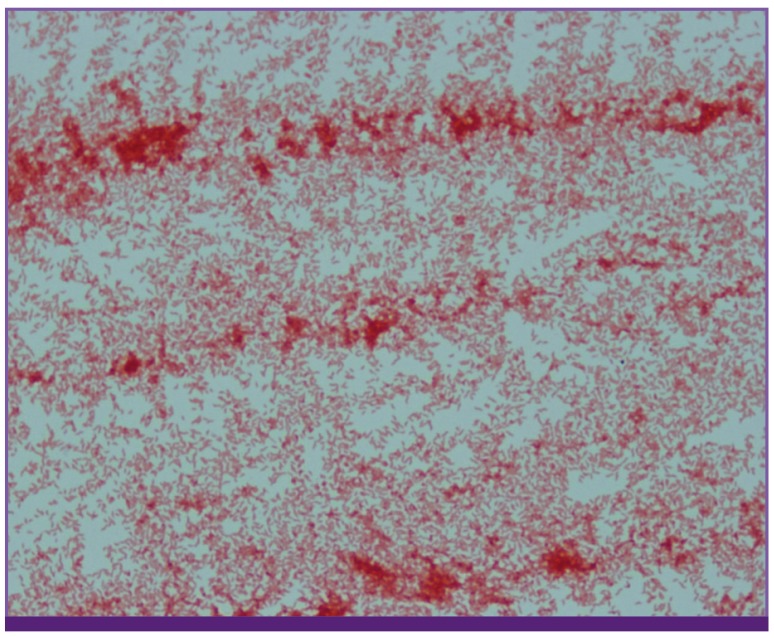
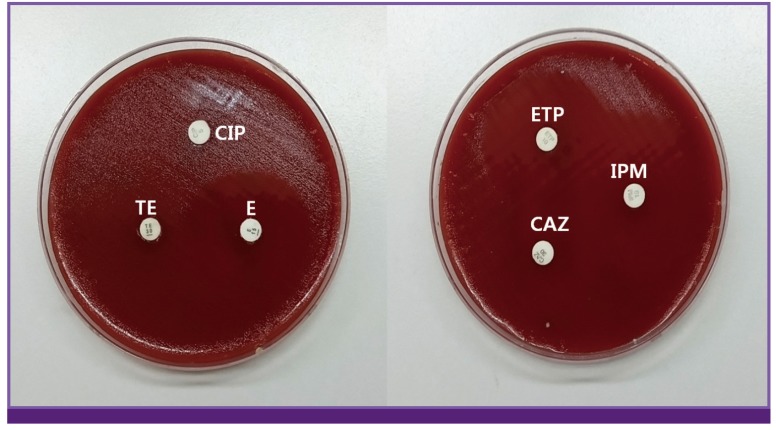
- Campylobacter infection causes gastrointestinal symptoms such as abdominal pain or diarrhea. Occasionally, Campylobacter bacteremia affects immunocompromised patients; however, serious outcomes are known to be rare. Here, we present a case of a patient with Campylobacter bacteremia who had underlying liver cirrhosis. The patient had fever and diarrhea. These symptoms subsided after treatment with cefotaxime. Campylobacter jejuni was isolated in the blood culture after 10 days. In addition, previously reported cases of Campylobacter bacteremia in Asian countries were reviewed with respect to antimicrobial sensitivities.
Keyword
MeSH Terms
Figure
Reference
-
1. Mori T, Hasegawa N, Sugita K, Shinjoh M, Nakamoto N, Shimizu T, Hori S, Iketani O, Fujiwara H, Takano Y, Iwata S. Clinical features of bacteremia due to Campylobacter jejuni . Intern Med. 2014; 53:1941–1944. PMID: 25175126.2. The European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters. Version 5.0, 2015. Accessed 30 June 2015. Available at: http://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_5.0_Breakpoint_Table_01.pdf.3. Scallan E, Hoekstra RM, Angulo FJ, Tauxe RV, Widdowson MA, Roy SL, Jones JL, Griffin PM. Foodborne illness acquired in the United States--major pathogens. Emerg Infect Dis. 2011; 17:7–15. PMID: 21192848.
Article4. Korea Centers for Disease Control and Prevention (KCDC). Epidemiological investigation of infectious diseases in Korea annual report 2013. Osong: KCDC;2014.5. Allos BM, Blaser MJ. Campylobacter jejuni and related species. In : Mandell GL, Bennet JE, Dolin R, editors. Mandell, Douglas, and Bennett's principles and practice of infectious diseases. 7th ed. Philadelphia, PA: Churchill Livingstone Elsevier;2010. p. 2793–2802.6. Yamagami K, Miyashita T, Nakamura T, Shirano M, Nakamura T, Kameda K, Nishijima M, Imanishi M, Yang X, Kanegane H. Campylobacter fetus bacteremia with purulent pleurisy in a young adult with primary hypogammaglobulinemia. Intern Med. 2014; 53:1221–1225. PMID: 24881753.7. Suzuki J, Sugiyama T, Ito K, Hadano Y, Kawamura I, Okinaka K, Kurai H, Ohkusu K, Ohmagari N. Campylobacter showae bacteremia with cholangitis. J Infect Chemother. 2013; 19:960–963. PMID: 23183773.8. Morishita S, Fujiwara H, Murota H, Maeda Y, Hara A, Horii T. Bloodstream infection caused by Campylobacter lari . J Infect Chemother. 2013; 19:333–337. PMID: 22965843.9. Liao CH, Chuang CY, Huang YT, Lee PI, Hsueh PR. Bacteremia caused by antimicrobial resistant Campylobacter species at a medical center in Taiwan, 1998-2008. J Infect. 2012; 65:392–399. PMID: 22771419.10. Abe I, Nomura M, Watanabe M, Shimada S, Kohno M, Matsuda Y, Adachi M, Kawate H, Ohnaka K, Takayanagi R. Pheochromocytoma crisis caused by Campylobacter fetus . Int J Urol. 2012; 19:465–467. PMID: 22221008.11. Shimizu Y, Ishii A, Takahata A, Kajiyama T, Yamahatsu A, Io H, Kurusu A, Hamada C, Horikoshi S, Tomino Y. Campylobacter bacteremia in hemodialysis patients by eating raw meat - the importance of sanitary education. Case Rep Nephrol Urol. 2012; 2:145–151. PMID: 23197970.12. Lang CL, Chiang CK, Hung KY, Wu KD. Campylobacter jejuni peritonitis and bacteremia in a patient undergoing continuous ambulatory peritoneal dialysis. Clin Nephrol. 2009; 71:96–98. PMID: 19203559.13. Okada H, Kitazawa T, Harada S, Itoyama S, Hatakeyama S, Ota Y, Koike K. Combined treatment with oral kanamycin and parenteral antibiotics for a case of persistent bacteremia and intestinal carriage with Campylobacter coli . Intern Med. 2008; 47:1363–1366. PMID: 18628588.14. Arai A, Kitano A, Sawabe E, Kanegane H, Miyawaki T, Miura O. Relapsing Campylobacter coli bacteremia with reactive arthritis in a patient with X-linked agammaglobulinemia. Intern Med. 2007; 46:605–609. PMID: 17473499.15. Jirapongsananuruk O, Wanotayan K, Phongsamart W, Chokephaibulkit K, Visitsunthorn N, Luangwedchakarn V, Vanprapar N, Vichyanond P. Recurrent Campylobacter lari bacteremia in X-linked agammaglobulinemia: a case report and review. Asian Pac J Allergy Immunol. 2006; 24:171–174. PMID: 17136884.16. Teh HS, Chiang SH, Tan AG, Sng LH, Oh HM. A case of right loin pain: septic ovarian vein thrombosis due to Campylobacter fetus bacteraemia. Ann Acad Med Singapore. 2004; 33:385–388. PMID: 15175788.17. Chuman Y, Takata T, Sameshima H, Takeuchi S, Takatsuka Y, Makino T, Blaser MJ, Utsunomiya A. Campylobacter fetus bacteremia in a patient with adult T cell leukemia. Clin Infect Dis. 2003; 36:1497–1498. PMID: 12766848.18. Woo PC, Leung KW, Tsoi HW, Wong SS, Teng JL, Yuen KY. Thermo-tolerant Campylobacter fetus bacteraemia identified by 16S ribosomal RNA gene sequencing: an emerging pathogen in immunocompromised patients. J Med Microbiol. 2002; 51:740–746. PMID: 12358064.19. National Committee on Clinical Laboratory Standards (NCCLS). Performance standard for antimicrobial disk susceptibility tests, 6th ed. approved standard M2-A6. Wayne, PA: NCCLS;1997.20. Cho IJ, Yim J, Lee Y, Kim MS, Seo Y, Chung HS, Yong D, Jeong SH, Lee K, Chong Y. Trends in isolation and antimicrobial susceptibility of enteropathogenic bacteria in 2001-2010 at a Korean tertiary care hospital. Ann Clin Microbiol. 2013; 16:45–51.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Campylobacter jejuni Bacteremia in a Healthy Child
- Two Cases of Campylobacter jejuni Bacteremia from Patients with Diarrhea
- A Septic Abortion Caused by Campylobacter jejuni bacteremia
- A Case of Campylobacter jejuni Enterocolitis with Acute Pancreatitis and Hemolytic Uremic Syndrome
- A Case of Campylobacter upsaliensis Bacteremia