J Korean Soc Surg Hand.
2017 Sep;22(3):147-153. 10.12790/jkssh.2017.22.3.147.
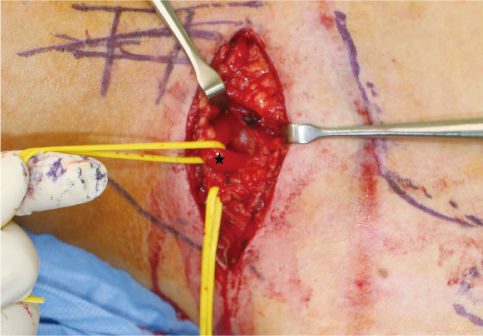
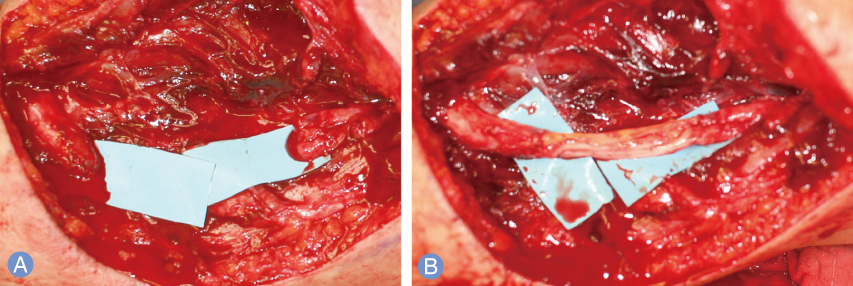
Nerve Repair and Nerve Grafting in Brachial Plexus Injuries
- Affiliations
-
- 1Department of Orthopedic Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. orth4535@gmail.com
- KMID: 2391211
- DOI: http://doi.org/10.12790/jkssh.2017.22.3.147
Abstract
- Brachial plexus injuries (BPI) can have devastating effects on upper extremity function, however, treatment in this injuries remains a difficult problem. Several kinds of surgical methods have been used to treat BPI, and nerve repair and nerve grafting have been traditionally used in postganglionic injury of brachial plexus. Because the several studies reported that nerve transfer to restore shoulder and elbow function has yielded superior results to historical reports for nerve grafting in partial BPI, the indication of nerve repair and nerve grafting has been decreased. Nonetheless, nerve repair and nerve grafting is still useful in focal damage in brachial plexus, such as laceration or gunshot wound and postganglionic neuroma in continuity without conduction of nerve action potential. In this paper, we described the basic concept, detailed indication and outcomes of nerve repair or nerve grafting in BPI.
Keyword
MeSH Terms
Figure
Reference
-
1. Sulaiman OA, Kim DD, Burkett C, Kline DG. Nerve transfer surgery for adult brachial plexus injury: a 10-year experience at Louisiana State University. Neurosurgery. 2009; 65:4 Suppl. A55–A62.2. Yang LJ, Chang KW, Chung KC. A systematic review of nerve transfer and nerve repair for the treatment of adult upper brachial plexus injury. Neurosurgery. 2012; 71:417–429.
Article3. Merrell GA, Barrie KA, Katz DL, Wolfe SW. Results of nerve transfer techniques for restoration of shoulder and elbow function in the context of a meta-analysis of the English literature. J Hand Surg Am. 2001; 26:303–314.
Article4. Furey MJ, Midha R, Xu QG, Belkas J, Gordon T. Prolonged target deprivation reduces the capacity of injured motoneurons to regenerate. Neurosurgery. 2007; 60:723–732.
Article5. Navarro X, Vivo M, Valero-Cabre A. Neural plasticity after peripheral nerve injury and regeneration. Prog Neurobiol. 2007; 82:163–201.
Article6. Kato S, Ide C. Axonal sprouting at the node of Ranvier of the peripheral nerve disconnected with the cell body. Restor Neurol Neurosci. 1994; 6:181–187.
Article7. Fried K, Govrin-Lippmann R, Rosenthal F, Ellisman MH, Devor M. Ultrastructure of afferent axon endings in a neuroma. J Neurocytol. 1991; 20:682–701.
Article8. Mohler LR, Hanel DP. Closed fractures complicated by peripheral nerve injury. J Am Acad Orthop Surg. 2006; 14:32–37.
Article9. Griffin JW, Hogan MV, Chhabra AB, Deal DN. Peripheral nerve repair and reconstruction. J Bone Joint Surg Am. 2013; 95:2144–2151.
Article10. Sunderland S. Factors influencing the course of regeneration and the quality of the recovery after nerve suture. Brain. 1952; 75:19–54.
Article11. Brophy RH, Wolfe SW. Planning brachial plexus surgery: treatment options and priorities. Hand Clin. 2005; 21:47–54.
Article12. Magalon G, Bordeaux J, Legre R, Aubert JP. Emergency versus delayed repair of severe brachial plexus injuries. Clin Orthop Relat Res. 1988; (237):32–35.
Article13. Bentolila V, Nizard R, Bizot P, Sedel L. Complete traumatic brachial plexus palsy. Treatment and outcome after repair. J Bone Joint Surg Am. 1999; 81:20–28.
Article14. Spinner RJ, Shin AY. Traumatic brachial plexus injury. In : Wolfe SW, Hotchkiss RN, Pederson WC, Kozin SH, Cohen MS, editors. Green's operative hand surgery. Philadelphia: Elsevier;2017. p. 1146–1207.15. Sedel L. The results of surgical repair of brachial plexus injuries. J Bone Joint Surg Br. 1982; 64:54–66.
Article16. Yamada S, Lonser RR, Iacono RP, Morenski JD, Bailey L. Bypass coaptation procedures for cervical nerve root avulsion. Neurosurgery. 1996; 38:1145–1151.
Article17. Malessy MJ, van Duinen SG, Feirabend HK, Thomeer RT. Correlation between histopathological findings in C-5 and C-6 nerve stumps and motor recovery following nerve grafting for repair of brachial plexus injury. J Neurosurg. 1999; 91:636–644.
Article18. Haninec P, Samal F, Tomas R, Houstava L, Dubovwy P. Direct repair (nerve grafting), neurotization, and end-to-side neurorrhaphy in the treatment of brachial plexus injury. J Neurosurg. 2007; 106:391–399.
Article19. Ali ZS, Heuer GG, Faught RW, et al. Upper brachial plexus injury in adults: comparative effectiveness of different repair techniques. J Neurosurg. 2015; 122:195–201.
Article20. Garg R, Merrell GA, Hillstrom HJ, Wolfe SW. Comparison of nerve transfers and nerve grafting for traumatic upper plexus palsy: a systematic review and analysis. J Bone Joint Surg Am. 2011; 93:819–829.
Article21. Chen L, Gu YD. An experimental study of contralateral C7 root transfer with vascularized nerve grafting to treat brachial plexus root avulsion. J Hand Surg Br. 1994; 19:60–66.
Article22. Terzis JK, Kostopoulos VK. Vascularized ulnar nerve graft: 151 reconstructions for posttraumatic brachial plexus palsy. Plast Reconstr Surg. 2009; 123:1276–1291.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intercostal nerve transfer for the treatment of brachial plexus injury
- Phrenic nerve palsy following coracoid infraclavicular brachial plexus block
- The Surgical Management of the Brachial Plexus Injuries: Report of 4 Among 7 Cases
- A Case of Neurilemmoma of the Brachial Plexus
- Electrical Stimulation for Early Axonal Regeneration after Nerve Surgery in Brachial Plexus Injury