Korean J Crit Care Med.
2017 Aug;32(3):291-294. 10.4266/kjccm.2016.00052.
Clozapine Induced Neuroleptic Malignant Syndrome
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- 2Division of Nephrology, Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. ohchris@hanmail.net
- 3Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2391189
- DOI: http://doi.org/10.4266/kjccm.2016.00052
Abstract
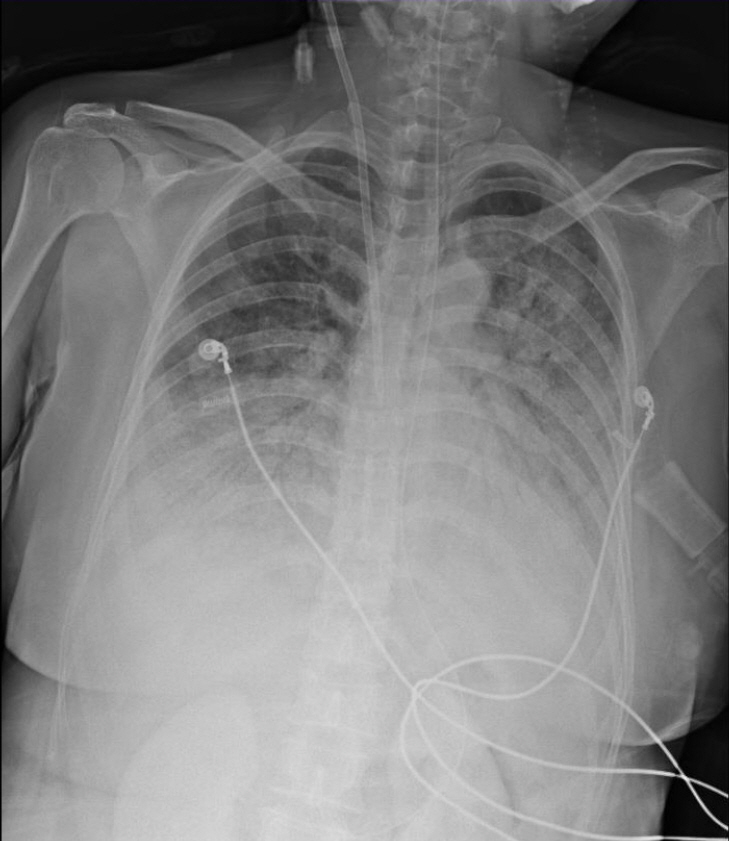
- Neuroleptic malignant syndrome is a rare, but potentially life-threatening adverse event associated with the use of neuroleptic agents. We describe the case of a 47-year-old schizophrenic woman who was treated with clozapine for years. The patient developed acute renal failure with pulmonary edema, and underwent mechanical ventilation and hemodialysis.
MeSH Terms
Figure
Reference
-
References
1. Delay J, Pichot P, Lemperiere T, Elissalde B, Peigne F. A non-phenothiazine and non-reserpine major neuroleptic, haloperidol, in the treatment of psychoses. Ann Med Psychol (Paris). 1960; 118:145–52.2. Tse L, M Barr AM, Scarapicchia V, Vila-Rodriguez F. Neuroleptic malignant syndrome: a review from a clinically oriented perspective. Curr Neuropharmacol. 2015; 13:395–406.
Article3. Shalev A, Hermesh H, Munitz H. Mortality from neuroleptic malignant syndrome. J Clin Psychiatry. 1989; 50:18–25.4. Caroff SN, Mann SC. Neuroleptic malignant syndrome. Med Clin North Am. 1993; 77:185–202.
Article5. Strawn JR, Keck PE Jr, Caroff SN. Neuroleptic malignant syndrome. Am J Psychiatry. 2007; 164:870–6.
Article6. Seitz DP, Gill SS. Neuroleptic malignant syndrome complicating antipsychotic treatment of delirium or agitation in medical and surgical patients: case reports and a review of the literature. Psychosomatics. 2009; 50:8–15.
Article7. Berardi D, Amore M, Keck PE Jr, Troia M, Dell’Atti M. Clinical and pharmacologic risk factors for neuroleptic malignant syndrome: a case-control study. Biol Psychiatry. 1998; 44:748–54.
Article8. Keck PE Jr, Pope HG Jr, Cohen BM, McElroy SL, Nierenberg AA. Risk factors for neuroleptic malignant syndrome. A case-control study. Arch Gen Psychiatry. 1989; 46:914–8.9. Pope HG Jr, Aizley HG, Keck PE Jr, McElroy SL. Neuroleptic malignant syndrome: long-term follow-up of 20 cases. J Clin Psychiatry. 1991; 52:208–12.10. Adnet P, Lestavel P, Krivosic-Horber R. Neuroleptic malignant syndrome. Br J Anaesth. 2000; 85:129–35.
Article11. Levenson JL. Neuroleptic malignant syndrome. Am J Psychiatry. 1985; 142:1137–45.12. Amore M, Montanari M. Neuroleptic malignant syndrome and related conditions. Minerva Psichiatr. 1992; 33:259–83.13. Velamoor VR, Norman RM, Caroff SN, Mann SC, Sullivan KA, Antelo RE. Progression of symptoms in neuroleptic malignant syndrome. J Nerv Ment Dis. 1994; 182:168–73.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Eosinophilia Induced by Clozapine
- Treatment of Clozapine-Induced Agranulocytosis Associated with Complications
- A Case of Atypical Neuroleptic Malignant Syndrome following Rebound Psychosis during Withdrawal of Clozapine
- A Case of Delayed Risperidone-induced Neuroleptic Malignant Syndrome
- A Case of Risperidone-induced Neuroleptic Malignant Syndrome