Electrolyte Blood Press.
2017 Sep;15(1):17-22. 10.5049/EBP.2017.15.1.17.
Renal Tubular Acidosis in Patients with Primary Sjögren's Syndrome
- Affiliations
-
- 1Department of Medicine, Graduate School, Kyung Hee University, Seoul, Korea.
- 2Division of Nephrology, Department of Internal Medicine, Kyung Hee University Medical Center, Seoul, Korea. khjeong@khu.ac.kr
- 3Divison of Nephrology, Department of Internal Medicine, Kyung Hee University Hospital at Gangdong, Seoul, Korea.
- KMID: 2391008
- DOI: http://doi.org/10.5049/EBP.2017.15.1.17
Abstract
- Primary Sjögren's syndrome (pSS) is characterized by lymphocytic infiltration of the exocrine glands resulting in decreased saliva and tear production. It uncommonly involves the kidneys in various forms, including tubulointerstitial nephritis, renal tubular acidosis, Fanconi syndrome, and rarely glomerulonephritis. Its clinical symptoms include muscle weakness, periodic paralysis, and bone pain due to metabolic acidosis and electrolyte imbalance. Herein, we describe the cases of two women with pSS whose presenting symptoms involve the kidneys. They had hypokalemia and normal anion gap metabolic acidosis due to distal renal tubular acidosis and positive anti-SS-A and anti-SS-B autoantibodies. Since one of them experienced femoral fracture due to osteomalacia secondary to renal tubular acidosis, an earlier diagnosis of pSS is important in preventing serious complications.
MeSH Terms
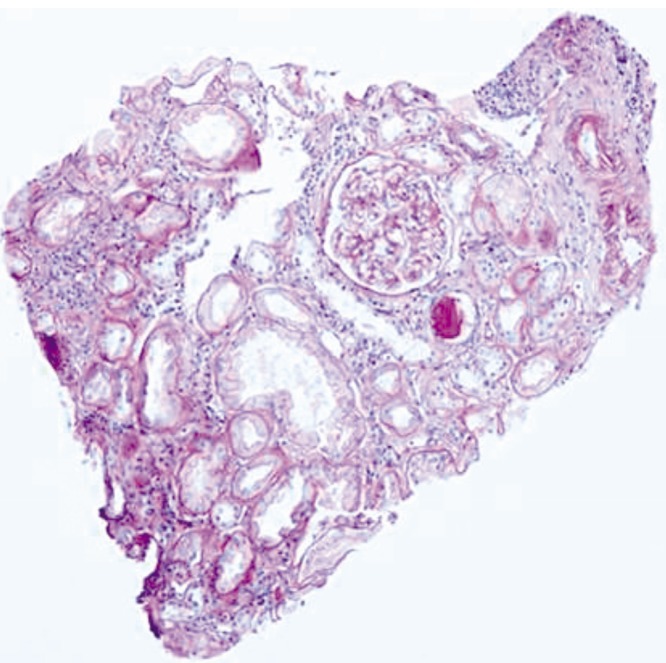
Figure
Reference
-
1. Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson JL, Loscalzo J. Harrison's principles of internal medicine. Sjögren's Syndrome. 18th ed. New York: McGraw-Hill;2012. p. 2770–2773.2. Goules AV, Tatouli IP, Moutsopoulos HM, Tzioufas AG. Clinically significant renal involvement in primary Sjogren's syndrome: clinical presentation and outcome. Arthritis Rheum. 2013; 65:2945–2953. PMID: 24166794.3. Seror R, Ravaud P, Bowman SJ, et al. EULAR Sjogren's syndrome disease activity index: development of a consensus systemic disease activity index for primary Sjogren's syndrome. Ann Rheum Dis. 2010; 69:1103–1109. PMID: 19561361.4. Francois H, Mariette X. Renal involvement in primary Sjogren syndrome. Nat Rev Nephrol. 2016; 12:82–93. PMID: 26568188.5. Yilmaz H, Kaya M, Ozbek M, K UU, Safa Yildirim I. Hypokalemic periodic paralysis in Sjogren's syndrome secondary to distal renal tubular acidosis. Rheumatol Int. 2013; 33:1879–1882. PMID: 22212410.
Article6. Han JS, Kim GH, Kim J, et al. Secretory-defect distal renal tubular acidosis is associated with transporter defect in H(+)-ATPase and anion exchanger-1. J Am Soc Nephrol. 2002; 13:1425–1432. PMID: 12039970.
Article7. Walsh S, Turner CM, Toye A, et al. Immunohistochemical comparison of a case of inherited distal renal tubular acidosis (with a unique AE1 mutation) with an acquired case secondary to autoimmune disease. Nephrol Dial Transplant. 2007; 22:807–812. PMID: 17205967.
Article8. Kim HY, Kim SS, Bae EH, Ma SK, Kim SW. Decreased Renal Expression of H(+)-ATPase and Pendrin in a Patient with Distal Renal Tubular Acidosis Associated with Sjogren's Syndrome. Intern Med. 2015; 54:2899–2904. PMID: 26568006.9. Khandelwal D, Bhattacharya S, Gadodia A, Khadgawat R, Tandon N, Ammini AC. Metabolic bone disease as a presenting manifestation of primary Sjogren's syndrome: Three cases and review of literature. Indian J Endocrinol Metab. 2011; 15:341–345. PMID: 22029009.10. Shane E, Burr D, Abrahamsen B, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014; 29:1–23. PMID: 23712442.
Article11. Fulop M, Mackay M. Renal tubular acidosis, Sjogren syndrome, and bone disease. Arch Intern Med. 2004; 164:905–909. PMID: 15111378.12. Geng Y, Zhao Y, Zhang Z. Tubulointerstitial nephritis-induced hypophosphatemic osteomalacia in Sjogren's syndrome: a case report and review of the literature. Clin Rheumatol. 2017.13. Vitali C, Bombardieri S, Jonsson R, et al. Classification criteria for Sjogren's syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Ann Rheum Dis. 2002; 61:554–558. PMID: 12006334.
Article14. Maripuri S, Grande JP, Osborn TG, et al. Renal involvement in primary Sjogren's syndrome: a clinicopathologic study. Clin J Am Soc Nephrol. 2009; 4:1423–1431. PMID: 19679669.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Distal Renal Tubular Acidosis with Sjögren's Syndrome Presenting as Hypokalemic Paralysis
- A Case of Primary Sjiigren's Syndrome with Hypokalemic Paralysis and Renal Tubular Acidosis
- Distal Renal Tubular Acidosis with Nephrocalcinosis in a Patient with Primary Sjogren's Syndrome
- A Case of Treatment with Steroid and Hydrochloroquine of Thrombocytopenia in Primary Sjögren's Syndrome
- A Case of Primary Sjorgen's Syndrome Presenting as Hypokalemic Periodic Paralysis