Chonnam Med J.
2017 Sep;53(3):203-210. 10.4068/cmj.2017.53.3.203.
Identification of Risk Factors Influencing In-Stent Restenosis with Acute Coronary Syndrome Presentation
- Affiliations
-
- 1Department of Cardiovascular Medicine, Regional Cardiocerebrovascular Center, Wonkang University Hospital, Iksan, Korea. librato46@gmail.com
- KMID: 2390434
- DOI: http://doi.org/10.4068/cmj.2017.53.3.203
Abstract
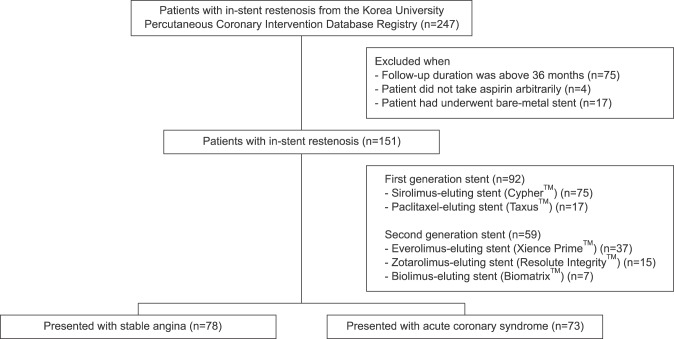
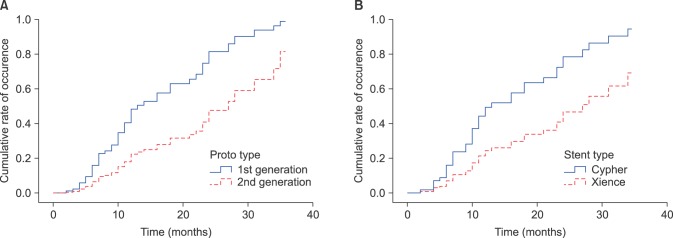
- Although the angiographic rates of in-stent restenosis (ISR) at later months have reduced dramatically with the introduction of drug-eluting stents (DESs), some patients with ISR after implantation of DES present with acute coronary syndrome (ACS). Here, we sought to identify parameters influencing the likelihood of restenosis with ACS presentation after DES implantation. Stented patients (n=3,817) with DESs in the Korea University Anam Hospital percutaneous coronary intervention registry were reviewed retrospectively for inclusion. In this database, 247 age- and sex-matched patients (6.5%) with ISR were allocated to either the Stable ISR group (n=78) or the ACS ISR group (n=73). Predictors of in-stent restenosis were identified with Cox regression analyses. Age (hazard ratio [HR], 1.14; 95% confidence interval [CI], 1.02 to 1.27; p=0.026), diabetes (HR, 8.40; 95% CI, 1.30 to 54.1; p=0.025), use of aspirin (HR, 0.003; 95% CI, 0.0001 to 0.63; p=0.03), clopidogrel (HR, 0.005; 95% CI, 0.001 to 0.121; p=0.001), renin-angiotensin system (RAS) blocker (HR, 0.02; 95% CI, 0.003 to 0.14; p<0.001), use of first -generation DES (HR, 0.07; 95% CI, 0.009 to 0.59; p=0.014), and matrix metalloproteinase 2 (MMP-2) levels (HR, 1.120; 95% CI, 1.001 to 1.190; p=0.004) during follow-up angiograms were significant predictors of ISR with ACS presentation during the 3 year follow-up. Age, diabetes, the use of first generation DES, and increased MMP-2 levels were significant predictors of ISR with ACS presentation; moreover, the use of aspirin, clopidogrel, RAS blocker, and the use of second generation DESs prevented ISR with ACS presentation.
Keyword
MeSH Terms
Figure
Reference
-
1. Kastrati A, Dibra A, Mehilli J, Mayer S, Pinieck S, Pache J, et al. Predictive factors of restenosis after coronary implantation of sirolimus- or paclitaxel-eluting stents. Circulation. 2006; 113:2293–2300. PMID: 16682614.2. Kastrati A, Schömig A, Elezi S, Schühlen H, Dirschinger J, Hadamitzky M, et al. Predictive factors of restenosis after coronary stent placement. J Am Coll Cardiol. 1997; 30:1428–1436. PMID: 9362398.3. Mishkel GJ, Moore AL, Markwell S, Shelton MC, Shelton ME. Long-term outcomes after management of restenosis or thrombosis of drug-eluting stents. J Am Coll Cardiol. 2007; 49:181–184. PMID: 17222728.4. Jørgensen B, Simonsen S, Endresen K, Forfang K, Vatne K, Hansen J, et al. Restenosis and clinical outcome in patients treated with amlodipine after angioplasty: results from the Coronary AngioPlasty Amlodipine REStenosis Study (CAPARES). J Am Coll Cardiol. 2000; 35:592–599. PMID: 10716459.5. Ribichini F, Wijns W, Ferrero V, Matullo G, Camilla T, Feola M, et al. Effect of angiotensin-converting enzyme inhibition on restenosis after coronary stenting. Am J Cardiol. 2003; 91:154–158. PMID: 12521626.6. Serruys PW, Foley DP, Jackson G, Bonnier H, Macaya C, Vrolix M, et al. A randomized placebo-controlled trial of fluvastatin for prevention of restenosis after successful coronary balloon angioplasty; final results of the fluvastatin angiographic restenosis (FLARE) trial. Eur Heart J. 1999; 20:58–69. PMID: 10075142.7. Rogers WJ, Canto JG, Lambrew CT, Tiefenbrunn AJ, Kinkaid B, Shoultz DA, et al. Temporal trends in the treatment of over 1.5 million patients with myocardial infarction in the US from 1990 through 1999: the National Registry of Myocardial Infarction 1, 2 and 3. J Am Coll Cardiol. 2000; 36:2056–2063. PMID: 11127441.8. Magalhaes MA, Minha S, Chen F, Torguson R, Omar AF, Loh JP, et al. Clinical presentation and outcomes of coronary in-stent restenosis across 3-stent generations. Circ Cardiovasc Interv. 2014; 7:768–776. PMID: 25466551.9. Assali AR, Moustapha A, Sdringola S, Denktas AE, Willerson JT, Holmes DR Jr, et al. Acute coronary syndrome may occur with in-stent restenosis and is associated with adverse outcomes (the PRESTO trial). Am J Cardiol. 2006; 98:729–733. PMID: 16950172.10. Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE Jr, et al. 2012 ACCF/AHA focused update incorporated into the ACCF/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013; 127:e663–e828. PMID: 23630129.11. O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013; 127:529–555. PMID: 23247303.12. Kai H, Ikeda H, Yasukawa H, Kai M, Seki Y, Kuwahara F, et al. Peripheral blood levels of matrix metalloproteases-2 and -9 are elevated in patients with acute coronary syndromes. J Am Coll Cardiol. 1998; 32:368–372. PMID: 9708462.13. Zeng B, Prasan A, Fung KC, Solanki V, Bruce D, Freedman SB, et al. Elevated circulating levels of matrix metalloproteinase-9 and -2 in patients with symptomatic coronary artery disease. Intern Med J. 2005; 35:331–335. PMID: 15892761.14. Baldus S, Heeschen C, Meinertz T, Zeiher AM, Eiserich JP, Münzel T, et al. Myeloperoxidase serum levels predict risk in patients with acute coronary syndromes. Circulation. 2003; 108:1440–1445. PMID: 12952835.15. Zhang R, Brennan ML, Fu X, Aviles RJ, Pearce GL, Penn MS, et al. Association between myeloperoxidase levels and risk of coronary artery disease. JAMA. 2001; 286:2136–2142. PMID: 11694155.16. Ikeda U, Ito T, Shimada K. Interleukin-6 and acute coronary syndrome. Clin Cardiol. 2001; 24:701–704. PMID: 11714126.17. Wang YN, Che SM, Ma AQ. Clinical significance of serum cytokines IL-1beta, sIL-2R, IL-6, TNF-alpha, and IFN-v in acute coronary syndrome. Chin Med Sci J. 2004; 19:120–124. PMID: 15250248.18. Nakamura Y, Shimada K, Fukuda D, Shimada Y, Ehara S, Hirose M, et al. Implications of plasma concentrations of adiponectin in patients with coronary artery disease. Heart. 2004; 90:528–533. PMID: 15084551.19. Otake H, Shite J, Shinke T, Watanabe S, Tanino Y, Ogasawara D, et al. Relation between plasma adiponectin, high-sensitivity C-reactive protein, and coronary plaque components in patients with acute coronary syndrome. Am J Cardiol. 2008; 101:1–7. PMID: 18157956.20. Mizia-Stec K, Gasior Z, Zahorska-Markiewicz B, Janowska J, Szulc A, Jastrzebska-Maj E, et al. Serum tumour necrosis factor-alpha, interleukin-2 and interleukin-10 activation in stable angina and acute coronary syndromes. Coron Artery Dis. 2003; 14:431–438. PMID: 12966263.21. Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol. 1983; 51:606. PMID: 6823874.22. Ellis SG, Vandormael MG, Cowley MJ, DiSciascio G, Deligonul U, Topol EJ, et al. Coronary morphologic and clinical determinants of procedural outcome with angioplasty for multivessel coronary disease. Implications for patient selection. Multivessel Angioplasty Prognosis Study Group. Circulation. 1990; 82:1193–1202. PMID: 2401060.23. Mehran R, Dangas G, Abizaid AS, Mintz GS, Lansky AJ, Satler LF, et al. Angiographic patterns of in-stent restenosis: classification and implications for long-term outcome. Circulation. 1999; 100:1872–1878. PMID: 10545431.24. Song HG, Kang SJ, Ahn JM, Kim WJ, Lee JY, Park DW, et al. Intravascular ultrasound assessment of optimal stent area to prevent in-stent restenosis after zotarolimus-, everolimus-, and sirolimus-eluting stent implantation. Catheter Cardiovasc Interv. 2014; 83:873–878. PMID: 22815193.25. Xu B, Yang Y, Yuan Z, Du Z, Wong SC, Généreux P, et al. Zotarolimus-and paclitaxel-eluting stents in an all-comer population in China: the RESOLUTE China randomized controlled trial. JACC Cardiovasc Interv. 2013; 6:664–670. PMID: 23523240.26. Kedhi E, Joesoef KS, McFadden E, Wassing J, van Mieghem C, Goedhart D, et al. Second-generation everolimus-eluting and paclitaxel-eluting stents in real-life practice (COMPARE): a randomised trial. Lancet. 2010; 375:201–209. PMID: 20060578.27. Hong SJ, Shim WJ, Choi JI, Joo HJ, Shin SY, Park SM, et al. Comparison of effects of telmisartan and valsartan on late lumen loss and inflammatory markers after sirolimus-eluting stent implantation in hypertensive patients. Am J Cardiol. 2007; 100:1625–1629. PMID: 18036359.28. Yoshida O, Hirayama H, Nanasato M, Watanabe T, Murohara T. The angiotensin II receptor blocker candesartan cilexetil reduces neointima proliferation after coronary stent implantation: a prospective randomized study under intravascular ultrasound guidance. Am Heart J. 2005; 149:e2. PMID: 15660025.29. Hotchi J, Hoshiga M, Takeda Y, Yuki T, Fujisaka T, Ishihara T, et al. Plaque-stabilizing effect of angiotensin-converting enzyme inhibitor and/or angiotensin receptor blocker in a rabbit plaque model. J Atheroscler Thromb. 2013; 20:257–266. PMID: 23154575.30. Morrissey RP, Diamond GA, Kaul S. Statins in acute coronary syndromes: do the guideline recommendations match the evidence? J Am Coll Cardiol. 2009; 54:1425–1433. PMID: 19796735.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Coronary Restenosis after Drug-Eluting Stent Implantation in Diabetic Patients
- Drug-Eluting Stent Used to Treat a Case of Recurrent Right Coronary Artery In-Stent Restenoses often Accompanied by Acute Inferior Wall Myocardial Infarction
- Drug-Eluting Stent Strut Fracture as a Cause of Restenosis
- Predictive Factors for Restenosis after Drug-Eluting Stent Implantation
- Clinical and Angiographic Factors Affect on In-Stent Restenosis