J Korean Med Sci.
2017 Nov;32(11):1870-1875. 10.3346/jkms.2017.32.11.1870.
The Clinical Differences between Urgent Visits and Non-Urgent Visits in Emergency Department During the Neonatal Period
- Affiliations
-
- 1Department of Emergency Medicine, Ajou University School of Medicine, Suwon, Korea. eesysook@naver.com
- 2Department of Emergency Medicine, Inje University Ilsan Paik Hospital, Goyang, Korea.
- 3Department of Preventive Medicine and Public Health, Ajou University School of Medicine, Suwon, Korea.
- KMID: 2390317
- DOI: http://doi.org/10.3346/jkms.2017.32.11.1870
Abstract
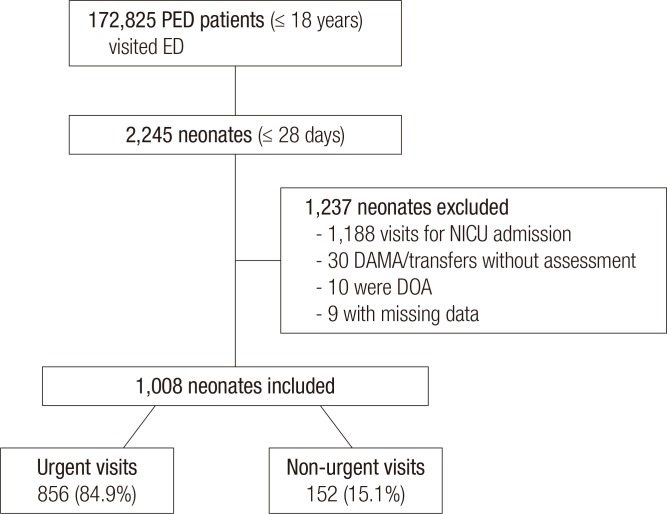
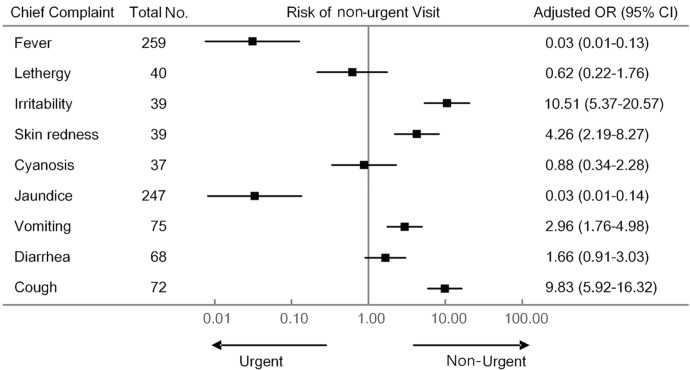
- As neonates are brought to the emergency department (ED) for various complaints, it is challenging for emergency physicians to clinically determine the urgency of the visit. We sought to explore clinical characteristics associated with urgent visits to the ED. We conducted a retrospective study by reviewing medical records of neonatal visits to a tertiary pediatric regional emergency center for 5 years. Cases of patients who were discharged after checking only chest or abdominal X-ray or discharged without workup, were classified as non-urgent visits. Cases where more examinations were performed, or when the patient was hospitalized, were classified as urgent visits. Various clinical features and process in the ED were compared between the groups. Of the 1,008 cases enrolled in this study, 856 (84.9%) were urgent and 152 (15.1%) were non-urgent visits. After adjustment by multiple logistic regression analysis, non-urgent visits were associated with self-referrals rather than physician-referrals (odds ratio [OR], 5.96), visits in the evening rather than at night or daytime (OR, 2.51), patient visits from home rather than from medical facilities (OR, 2.19; 95). Fever and jaundice were the most common complaints (25.7% and 24.5%, respectively), and their OR of non-urgent visit was relatively low (adjusted OR 0.03 and 0.03, respectively). However, other common complaints, such as vomiting and cough (7.4% and 7.1%, respectively), were more likely to be non-urgent visits (adjusted OR 2.96 and 9.83, respectively). For suspected non-urgent visits, emergency physicians need to try to reduce unnecessary workup and shorten length of stay in ED.
Keyword
MeSH Terms
Figure
Reference
-
1. Williams RM. The costs of visits to emergency departments. N Engl J Med. 1996; 334:642–646. PMID: 8592529.2. Bernstein SL, Aronsky D, Duseja R, Epstein S, Handel D, Hwang U, McCarthy M, John McConnell K, Pines JM, Rathlev N, et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009; 16:1–10. PMID: 19007346.3. Alpern ER, Stanley RM, Gorelick MH, Donaldson A, Knight S, Teach SJ, Singh T, Mahajan P, Goepp JG, Kuppermann N, et al. Epidemiology of a pediatric emergency medicine research network: the PECARN Core Data Project. Pediatr Emerg Care. 2006; 22:689–699.4. Brousseau T, Sharieff GQ. Newborn emergencies: the first 30 days of life. Pediatr Clin North Am. 2006; 53:69–84. vi.PMID: 16487785.5. Núñez S, Moreno A, Green K, Villar J. The stethoscope in the emergency department: a vector of infection? Epidemiol Infect. 2000; 124:233–237. PMID: 10813148.6. Phelps K, Taylor C, Kimmel S, Nagel R, Klein W, Puczynski S. Factors associated with emergency department utilization for nonurgent pediatric problems. Arch Fam Med. 2000; 9:1086–1092. PMID: 11115212.7. Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008; 52:126–136. PMID: 18433933.8. Kennedy TJ, Purcell LK, LeBlanc JC, Jangaard KA. Emergency department use by infants less than 14 days of age. Pediatr Emerg Care. 2004; 20:437–442. PMID: 15232243.9. Batu ED, Yeni S, Teksam O. The factors affecting neonatal presentations to the pediatric emergency department. J Emerg Med. 2015; 48:542–547. PMID: 25648054.10. Calado CS, Pereira AG, Santos VN, Castro MJ, Maio JF. What brings newborns to the emergency department?: a 1-year study. Pediatr Emerg Care. 2009; 25:244–248. PMID: 19382329.11. Boulvain M, Perneger TV, Othenin-Girard V, Petrou S, Berner M, Irion O. Home-based versus hospital-based postnatal care: a randomised trial. BJOG. 2004; 111:807–813. PMID: 15270928.12. Paul IM, Phillips TA, Widome MD, Hollenbeak CS. Cost-effectiveness of postnatal home nursing visits for prevention of hospital care for jaundice and dehydration. Pediatrics. 2004; 114:1015–1022. PMID: 15466099.13. Flanagan CF, Stewart M. Factors associated with early neonatal attendance to a paediatric emergency department. Arch Dis Child. 2014; 99:239–243. PMID: 24246192.14. Lain SJ, Nassar N, Bowen JR, Roberts CL. Risk factors and costs of hospital admissions in first year of life: a population-based study. J Pediatr. 2013; 163:1014–1019. PMID: 23769505.15. Lee HC, Bardach NS, Maselli JH, Gonzales R. Emergency department visits in the neonatal period in the United States. Pediatr Emerg Care. 2014; 30:315–318. PMID: 24759490.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Impact of an Emergency Fee Increase on the Composition of Patients Visiting Emergency Departments
- The Analysis of Emergency Department Costs
- The Impact of Middle East Respiratory Syndrome Outbreak on Trends in Emergency Department Utilization Patterns
- Coronavirus disease 2019 pandemic-related change in children’s visits to the emergency department
- Changes in pediatric injury-related visits during coronavirus disease 2019 pandemic at a single regional emergency medical center in Korea