Korean J Ophthalmol.
2017 Oct;31(5):439-445. 10.3341/kjo.2016.0090.
Short-term Analysis of the Residual Volume of an Eye Drop Following 23-Gauge Microincision Vitrectomy Surgery
- Affiliations
-
- 1Department of Ophthalmology, Kyungpook National University School of Medicine, Daegu, Korea. sarasate2222@gmail.com
- 2Department of Ophthalmology, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea.
- KMID: 2390287
- DOI: http://doi.org/10.3341/kjo.2016.0090
Abstract
- PURPOSE
To evaluate the change of residual volume of eye drop after instillation in patients with 23-gauge microincision vitrectomy surgery (MIVS).
METHODS
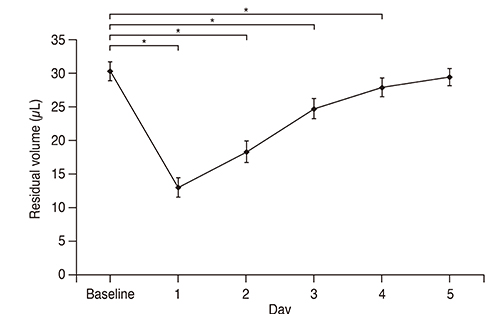
Patient who were treated 23-gauge MIVS from November 2014 to July 2015 were included. The residual volume was defined as the amount of remnant eye drop in patient's eyes after instillation, calculated as the difference between instillation volume and spilled volume of eye drop. Calculation of residual volume of eye drop was performed one day before surgery, and daily from postoperative day 1 to day 5.
RESULTS
Forty consecutive patients were included. The residual volume of eye drop decreased from 30.3 ± 1.4 µL at baseline to 13.0 ± 1.5 µL at day 1, 18.3 ± 1.6 µL at day 2, 24.7 ± 1.5 µL at day 3, and 27.9 ± 1.4 µL in day 4, postoperatively (p < 0.001, respectively). The volume at postoperative day 5 was 29.4 ± 1.3 µL, but it was not different from the volume at baseline (p = 0.105). The change of residual volume was significantly correlated with postoperative chemosis (r = 0.672, p < 0.001) and effected by the number of quadrant with postoperative chemosis (p < 0.05).
CONCLUSIONS
This study shows that postoperative residual volume of eye drop after instillation decreased until postoperative day 4, and postoperative chemosis affects the change of residual volume. Thus, checking proper use of eye drops and teaching about instillation technique by physician is necessary for patients with 23-gauge MIVS.
Keyword
Figure
Reference
-
1. Gaudana R, Ananthula HK, Parenky A, Mitra AK. Ocular drug delivery. AAPS J. 2010; 12:348–360.2. Olson RJ. Reducing the risk of postoperative endophthalmitis. Surv Ophthalmol. 2004; 49:Suppl 2. S55–S61.3. Androudi S, Ahmed M, Fiore T, et al. Combined pars plana vitrectomy and phacoemulsification to restore visual acuity in patients with chronic uveitis. J Cataract Refract Surg. 2005; 31:472–478.4. Winfield AJ, Jessiman D, Williams A, Esakowitz L. A study of the causes of non-compliance by patients prescribed eyedrops. Br J Ophthalmol. 1990; 74:477–480.5. Lund W, editor. The pharmaceutical codex: principles and practice of pharmaceutics. 12th ed. London: Pharmaceutical Press;1994. p. 14.6. File RR, Patton TF. Topically applied pilocarpine: human pupillary response as a function of drop size. Arch Ophthalmol. 1980; 98:112–115.7. Gray RH. The influence of drop size on pupil dilatation. Eye (Lond). 1991; 5(Pt 5):615–619.8. Craig EW, Griffiths PG. Effect on mydriasis of modifying the volume of phenylephrine drops. Br J Ophthalmol. 1991; 75:222–223.9. Tatham AJ, Sarodia U, Gatrad F, Awan A. Eye drop instillation technique in patients with glaucoma. Eye (Lond). 2013; 27:1293–1298.10. Costen MT, Newsom RS, Wainwright AC, et al. Expanding role of local anaesthesia in vitreoretinal surgery. Eye (Lond). 2005; 19:755–761.11. Barrio-Barrio J, Sabater AL, Bonet-Farriol E, Velazquez-Villoria A, Galofre JC. Graves' ophthalmopathy: VISA versus EUGOGO Classification, Assessment, and Management. J Ophthalmol. 2015; 2015:249125.12. Ritch R, Jamal KN, Gurses-Ozden R, Liebmann JM. An improved technique of eye drop self-administration for patients with limited vision. Am J Ophthalmol. 2003; 135:530–533.13. Brown MM, Brown GC, Spaeth GL. Improper topical self-administration of ocular medication among patients with glaucoma. Can J Ophthalmol. 1984; 19:2–5.14. Kholdebarin R, Campbell RJ, Jin YP, Buys YM. Multicenter study of compliance and drop administration in glaucoma. Can J Ophthalmol. 2008; 43:454–461.15. Lee SB, Lee DG, Kwag JY, Kim JY. The effect of mydriatics on posterior synechia after combined pars plana vitrectomy, phacoemulsification, and intraocular lens implantation. Retina. 2009; 29:1150–1154.16. Mishima S, Gasset A, Klyce SD Jr, Baum JL. Determination of tear volume and tear flow. Invest Ophthalmol. 1966; 5:264–276.17. Allansmith MR, Baird RS, Higgenbotham EJ, Abelson MB. Technical aspects of histamine determination in human tears. Am J Ophthalmol. 1980; 90:719–724.18. Jones DT, Monroy D, Pflugfelder SC. A novel method of tear collection: comparison of glass capillary micropipettes with porous polyester rods. Cornea. 1997; 16:450–458.19. Choy CK, Cho P, Chung WY, Benzie IF. Water-soluble antioxidants in human tears: effect of the collection method. Invest Ophthalmol Vis Sci. 2001; 42:3130–3134.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Short-term Changes in Ocular Surface pH after 23-gauge Microincision Vitrectomy Surgery
- Sclerotomy-related Retinal Breaks in Vitrectomy for Proliferative Diabetic Retinopathy: 20- vs 23-Gauge Systems
- The Clinical Results of Sutureless Vitrectomy Using 23-Gauge Surgical System
- Comparison of Surgically-induced Astigmatism after Combined Phacoemulsification and 23-Gauge Vitrectomy: 2.2-mm vs. 2.75-mm Cataract Surgery
- Complication Incidence of Day Surgeries with 23 Gauge Vitrectomy