Ann Rehabil Med.
2017 Apr;41(2):225-230. 10.5535/arm.2017.41.2.225.
Lesion Characteristics of Chronic Dysphagia in Patients With Supratentorial Stroke
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Veterans Health Service Medical Center, Seoul, Korea. hohoho7490@gmail.com
- KMID: 2389480
- DOI: http://doi.org/10.5535/arm.2017.41.2.225
Abstract
OBJECTIVE
To analyze the relationship between brain lesion location and type of chronic dysphagia in patients with supratentorial stroke.
METHODS
Data from 82 chronic stroke patients who underwent videofluoroscopic swallowing studies at >6 months after an initial stroke event were retrospectively analyzed. Delayed oral transit time, delayed pharyngeal transit time, and the presence of aspiration were extracted. A voxel-based lesion symptom mapping (VLSM) analysis was used to correlate types of dysphagia with specific brain lesions.
RESULTS
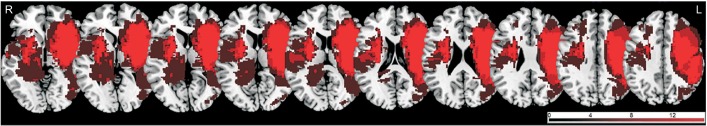
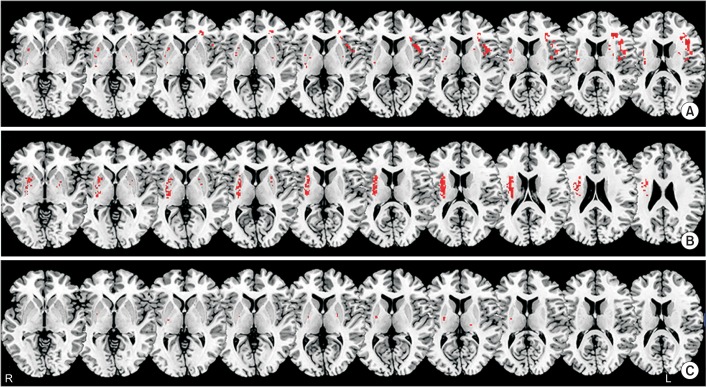
VLSM identified several clusters of voxels that significantly correlated with type of dysphagia. Delayed oral transit time mainly correlated with lesions in the left inferior frontal lobe and precentral gyrus; delayed pharyngeal time mainly correlated with lesions in the right basal ganglia and corona radiate; and aspiration was mainly correlated with lesions in the putamen.
CONCLUSION
Understanding the association between lesion location and dysphagia in chronic stroke patients is an important first step towards predicting permanent dysphagia after stroke. Improved understanding of the neural correlates of dysphagia will inform the utility of interventions for its treatment and prevention after stroke.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Association of Brain Lesions and Videofluoroscopic Dysphagia Scale Parameters on Patients With Acute Cerebral Infarctions
Sang Jun Mo, Ho Joong Jeong, Yong Hyun Han, Kihun Hwang, Jong Kyoung Choi
Ann Rehabil Med. 2018;42(4):560-568. doi: 10.5535/arm.2018.42.4.560.
Reference
-
1. Mann G, Hankey GJ, Cameron D. Swallowing disorders following acute stroke: prevalence and diagnostic accuracy. Cerebrovasc Dis. 2000; 10:380–386. PMID: 10971024.
Article2. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005; 36:2756–2763. PMID: 16269630.3. Han H, Shin G, Jun A, Park T, Ko D, Choi E, et al. The relation between the presence of aspiration or penetration and the clinical indicators of dysphagia in poststroke survivors. Ann Rehabil Med. 2016; 40:88–94. PMID: 26949674.
Article4. Steinhagen V, Grossmann A, Benecke R, Walter U. Swallowing disturbance pattern relates to brain lesion location in acute stroke patients. Stroke. 2009; 40:1903–1906. PMID: 19286597.
Article5. Daniels SK, Foundas AL, Iglesia GC, Sullivan MA. Lesion site in unilateral stroke patients with dysphagia. J Stroke Cerebrovasc Dis. 1996; 6:30–34. PMID: 17894962.
Article6. Galovic M, Leisi N, Muller M, Weber J, Abela E, Kagi G, et al. Lesion location predicts transient and extended risk of aspiration after supratentorial ischemic stroke. Stroke. 2013; 44:2760–2767. PMID: 23887840.
Article7. Daniels SK, Corey DM, Fraychinaud A, DePolo A, Foundas AL. Swallowing lateralization: the effects of modified dual-task interference. Dysphagia. 2006; 21:21–27. PMID: 16544089.
Article8. Logemann JA. Evaluation and treatment of swallowing disorders. 2nd ed. Austin: Pro-ED;1998.9. Rorden C, Karnath HO, Bonilha L. Improving lesion-symptom mapping. J Cogn Neurosci. 2007; 19:1081–1088. PMID: 17583985.
Article10. Picelli A, Tamburin S, Gajofatto F, Zanette G, Praitano M, Saltuari L, et al. Association between severe upper limb spasticity and brain lesion location in stroke patients. Biomed Res Int. 2014; 2014:162754. PMID: 24963473.
Article11. Rorden C, Bonilha L, Nichols TE. Rank-order versus mean based statistics for neuroimaging. Neuroimage. 2007; 35:1531–1537. PMID: 17391987.
Article12. Robbins J, Levine RL, Maser A, Rosenbek JC, Kempster GB. Swallowing after unilateral stroke of the cerebral cortex. Arch Phys Med Rehabil. 1993; 74:1295–1300. PMID: 8259895.
Article13. Horner J, Massey EW, Brazer SR. Aspiration in bilateral stroke patients. Neurology. 1990; 40:1686–1688. PMID: 2234422.
Article14. Dziewas R, Soros P, Ishii R, Chau W, Henningsen H, Ringelstein EB, et al. Neuroimaging evidence for cortical involvement in the preparation and in the act of swallowing. Neuroimage. 2003; 20:135–144. PMID: 14527576.
Article15. Martin RE, Sessle BJ. The role of the cerebral cortex in swallowing. Dysphagia. 1993; 8:195–202. PMID: 8359039.
Article16. Smithard DG, O'Neill PA, Parks C, Morris J. Complications and outcome after acute stroke. Does dysphagia matter? Stroke. 1996; 27:1200–1204. PMID: 8685928.17. Kidd D, Lawson J, Nesbitt R, MacMahon J. The natural history and clinical consequences of aspiration in acute stroke. QJM. 1995; 88:409–413. PMID: 7648232.18. Ertekin C. Voluntary versus spontaneous swallowing in man. Dysphagia. 2011; 26:183–192. PMID: 21161279.
Article19. Teismann IK, Dziewas R, Steinstraeter O, Pantev C. Time-dependent hemispheric shift of the cortical control of volitional swallowing. Hum Brain Mapp. 2009; 30:92–100. PMID: 17979116.
Article20. Watanabe Y, Abe S, Ishikawa T, Yamada Y, Yamane GY. Cortical regulation during the early stage of initiation of voluntary swallowing in humans. Dysphagia. 2004; 19:100–108. PMID: 15382798.
Article21. Daniels SK, Brailey K, Foundas AL. Lingual discoordination and dysphagia following acute stroke: analyses of lesion localization. Dysphagia. 1999; 14:85–92. PMID: 10028038.
Article22. Hamdy S, Aziz Q, Rothwell JC, Singh KD, Barlow J, Hughes DG, et al. The cortical topography of human swallowing musculature in health and disease. Nat Med. 1996; 2:1217–1224. PMID: 8898748.
Article23. Kwon M, Lee JH, Kim JS. Dysphagia in unilateral medullary infarction: lateral vs medial lesions. Neurology. 2005; 65:714–718. PMID: 16157904.
Article24. Cola MG, Daniels SK, Corey DM, Lemen LC, Romero M, Foundas AL. Relevance of subcortical stroke in dysphagia. Stroke. 2010; 41:482–486. PMID: 20093638.
Article25. Wan P, Chen X, Zhu L, Xu S, Huang L, Li X, et al. Dysphagia post subcortical and supratentorial stroke. J Stroke Cerebrovasc Dis. 2016; 25:74–82. PMID: 26508684.
Article26. Heilman KM, Van Den Abell T. Right hemisphere dominance for attention: the mechanism underlying hemispheric asymmetries of inattention (neglect). Neurology. 1980; 30:327–330. PMID: 7189037.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Dysphagia Between Infratentorial and Supratentorial Stroke Patients
- Epidemiology, Natural Recovery, Long-term Outcome of Post Stroke Dysphagia
- Relationship Between Cognitive Function and Dysphagia After Stroke
- Neuroanatomical Predictors of Dysphagia after Stroke: Voxel-Based Lesion Symptom Mapping Study
- Post-Stroke Dysphagia: Incidence, Complications and Pattern Relates to Brain Lesion