Ann Rehabil Med.
2017 Jun;41(3):413-420. 10.5535/arm.2017.41.3.413.
Contrast Spread in the Superoposterior Approach of Transforaminal Epidural Steroid Injections for Lumbosacral Radiculopathy
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Korea University Guro Hospital, Seoul, Korea. rehab46@korea.ac.kr
- KMID: 2389456
- DOI: http://doi.org/10.5535/arm.2017.41.3.413
Abstract
OBJECTIVE
To observe the contrast spread in superoposterior transforaminal epidural steroid injection (SP TFESI) and investigate the correlation between spread patterns and efficacy.
METHODS
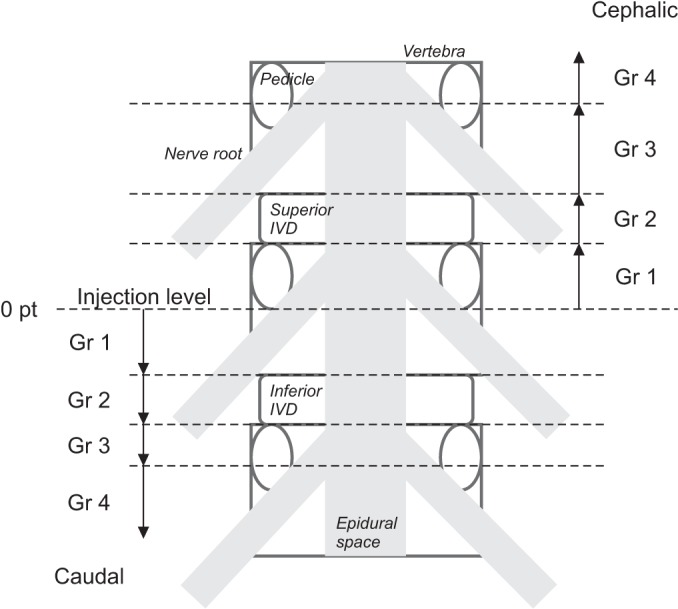
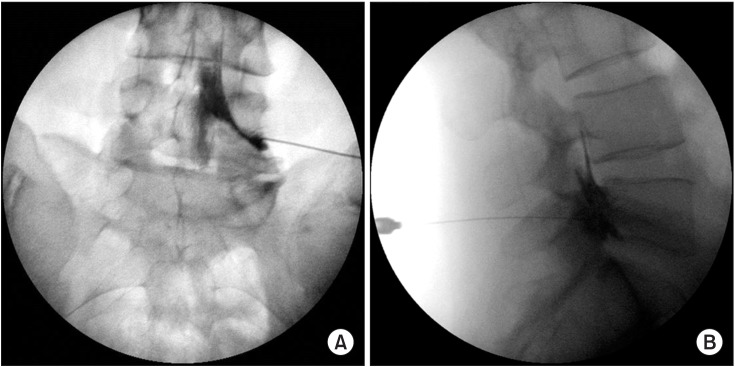
Thirty-one patients with lumbosacral radiculopathy underwent single-level TFESI under fluoroscopy. The final needle tip position was targeted toward the SP quadrant of the intervertebral foramen. To observe the spread, 1 mL of contrast material was injected, followed by a steroid injection. The contrast spread was graded anteroposteriorly and vertically in the epidural space. The effect of SP TFESI was evaluated by proportional pain score reduction.
RESULTS
Levels injected were L4-5 (n=20) and L5-S1 (n=11). Seventeen cases were lateral, and 14 were central herniated disc (HD). Baseline mean visual analog scale score was 6.23. Contrast dispersed dorsally in all the cases, and 45.2% cases showed a concurrent ventral spread. The proportion of the pain reduction after 2 weeks showed no difference between the two groups. In vertical spreading analysis, mean cephalic/caudal grades were 1.40/1.55 at L4-5 level and 1.73/1.64 at L5-S1 level. The HD location had no effect on contrast dispersion.
CONCLUSION
In SP TFESI, ventral contrast spread did not guarantee a better effect; however, the extent of cephalic flow in ventral expansion group correlated with the proportion of pain reduction.
MeSH Terms
Figure
Reference
-
1. Manchikanti L, Staats PS, Singh V, Schultz DM, Vilims BD, Jasper JF, et al. Evidence-based practice guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 2003; 6:3–81. PMID: 16878163.2. Boswell MV, Hansen HC, Trescot AM, Hirsch JA. Epidural steroids in the management of chronic spinal pain and radiculopathy. Pain Physician. 2003; 6:319–334. PMID: 16880879.3. Ackerman WE 3rd, Ahmad M. The efficacy of lumbar epidural steroid injections in patients with lumbar disc herniations. Anesth Analg. 2007; 104:1217–1222. PMID: 17456677.
Article4. Manchikanti L. Transforaminal lumbar epidural steroid injections. Pain Physician. 2000; 3:374–398. PMID: 16906179.
Article5. Lee IS, Kim SH, Lee JW, Hong SH, Choi JY, Kang HS, et al. Comparison of the temporary diagnostic relief of transforaminal epidural steroid injection approaches: conventional versus posterolateral technique. AJNR Am J Neuroradiol. 2007; 28:204–208. PMID: 17296980.6. Devereaux MW. Anatomy and examination of the spine. Neurol Clin. 2007; 25:331–351. PMID: 17445732.
Article7. Adamkiewicz A. Die blutgefasse des menschlichen ruckenmarkes. II Theil: Die gefasse der ruckenmarksoberflache. S B Heidelberg Akad Wiss. 1882; 85:101–130.8. Kirkaldy-Willis WH, Bernard TN. Managing low back pain. 4th ed. London: Churchill Livingstone;1999.9. Murthy NS, Maus TP, Behrns CL. Intraforaminal location of the great anterior radiculomedullary artery (artery of Adamkiewicz): a retrospective review. Pain Med. 2010; 11:1756–1764. PMID: 21134118.
Article10. Lyders EM, Morris PP. A case of spinal cord infarction following lumbar transforaminal epidural steroid injection: MR imaging and angiographic findings. AJNR Am J Neuroradiol. 2009; 30:1691–1693. PMID: 19369604.
Article11. Somayaji HS, Saifuddin A, Casey AT, Briggs TW. Spinal cord infarction following therapeutic computed tomography-guided left L2 nerve root injection. Spine (Phila Pa 1976). 2005; 30:E106–E108. PMID: 15706327.
Article12. Jasper JF. Lumbar retrodiscal transforaminal injection. Pain Physician. 2007; 10:501–510. PMID: 17525785.
Article13. Glaser SE, Shah RV. Root cause analysis of paraplegia following transforaminal epidural steroid injections: the ‘unsafe’ triangle. Pain Physician. 2010; 13:237–244. PMID: 20495587.14. Helm S, Glaser S, Falco F, Henry B. A medical-legal review regarding the standard of care for epidural injections, with particular reference to a closed case. Pain Physician. 2010; 13:145–150. PMID: 20309380.15. Desai MJ, Shah B, Sayal PK. Epidural contrast flow patterns of transforaminal epidural steroid injections stratified by commonly used final needle-tip position. Pain Med. 2011; 12:864–870. PMID: 21539705.
Article16. Fardon DF, Williams AL, Dohring EJ, Murtagh FR, Gabriel Rothman SL, Sze GK. Lumbar disc nomenclature: version 2.0: Recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology. Spine J. 2014; 14:2525–2545. PMID: 24768732.17. Vassiliev D. Spread of contrast during L4 and L5 nerve root infiltration under fluoroscopic guidance. Pain Physician. 2007; 10:461–466. PMID: 17525780.18. Ahn KH, Kim HS, Lee JH, Kim DH, Cho DI, Shin JC, et al. Effects of L4-5 transforaminal epidural steroid injection in L5 radiculopathy. J Korean Acad Rehabil Med. 2005; 29:281–285.19. Furman MB, Mehta AR, Kim RE, Simon JI, Patel R, Lee TS, et al. Injectate volumes needed to reach specific landmarks in lumbar transforaminal epidural injections. PM R. 2010; 2:625–635. PMID: 20659718.
Article20. Atluri S, Glaser SE, Shah RV, Sudarshan G. Needle position analysis in cases of paralysis from transforaminal epidurals: consider alternative approaches to traditional technique. Pain Physician. 2013; 16:321–334. PMID: 23877448.21. Lee HM, Kim NH, Kim HJ, Chung IH. Morphometric study of the lumbar spinal canal in the Korean population. Spine (Phila Pa 1976). 1995; 20:1679–1684. PMID: 7482017.
Article22. Botwin K, Natalicchio J, Brown LA. Epidurography contrast patterns with fluoroscopic guided lumbar transforaminal epidural injections: a prospective evaluation. Pain Physician. 2004; 7:211–215. PMID: 16868594.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Transforaminal Epidural Steroid Injection and Lumbar/Caudal Epidural Steroid Injection for the Treatment of Lumbosacral Radiculopathy
- Evaluation of Contrast Flow Patterns with Fluoroscopic Guided Lumbar Transforaminal Epidural Injections
- Contrast Spreading Patterns in Retrodiscal Transforaminal Epidural Steroid Injection
- Epidural Steroid Injection for Lumbosacral Radiculopathy
- Preganglionic Epidural Steroid Injection through Translateral Recess Approach