Ann Rehabil Med.
2017 Aug;41(4):631-637. 10.5535/arm.2017.41.4.631.
Verification of Reliability and Validity of the Feeding and Swallowing Scale for Premature Infants (FSSPI)
- Affiliations
-
- 1Department of Physical and Rehabilitation Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jeongyi.kwon@samsung.com
- KMID: 2389409
- DOI: http://doi.org/10.5535/arm.2017.41.4.631
Abstract
OBJECTIVE
To propose a new scale, the Feeding and Swallowing Scale for Premature Infants (FSSPI), based on videofluoroscopic swallowing study (VFSS) findings and to verify the reliability and validity of the FSSPI.
METHODS
One hundred thirty preterm infants who had undergone VFSS were enrolled in this retrospective study. The FSSPI was developed by referring to the Baby Regulated Organization of Subsystems and Sucking approach. The FSSPI score for each VFSS video was evaluated by a physiatrist as well as by three experienced speech-language pathologists. To verify the reliability of the FSSPI, the inter-evaluator and intra-evaluator associations for the FSSPI scores were analyzed. To verify the validity of the FSSPI, the association between FSSPI scores and clinical characteristics including prognosis-related factors was analyzed.
RESULTS
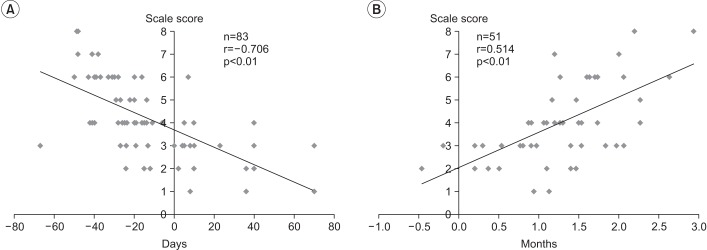
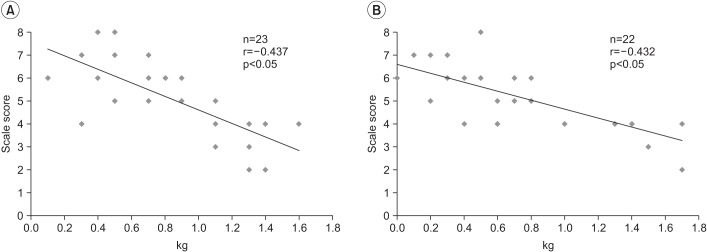
The mean gestational age was 27.3±2.8 weeks. The FSSPI showed a high degree of both intra-rater reliability and inter-rater reliability. Also, there was a significant negative correlation between the FSSPI score and corrected age (CA) at the time of performing VFSS. Further, a significant positive correlation was observed between the FSSPI score and CA at the time of achieving full oral feeding. A significant negative correlation was observed between the FSSPI score and weight gain, between the 1st and 2nd month after birth, and between the 2nd and 3rd month after birth, respectively.
CONCLUSION
In this study, we proposed a new clinical scale using VFSS to reflect the development of feeding and swallowing skills in preterm infants. Further, we verified the reliability and validity of the scale.
Keyword
MeSH Terms
Figure
Reference
-
1. Gewolb IH, Bosma JF, Taciak VL, Vice FL. Abnormal developmental patterns of suck and swallow rhythms during feeding in preterm infants with bronchopulmonary dysplasia. Dev Med Child Neurol. 2001; 43:454–459. PMID: 11463175.
Article2. Amaizu N, Shulman R, Schanler R, Lau C. Maturation of oral feeding skills in preterm infants. Acta Paediatr. 2008; 97:61–67.
Article3. Goldfield EC, Buonomo C, Fletcher K, Perez J, Margetts S, Hansen A, et al. Premature infant swallowing: patterns of tongue-soft palate coordination based upon videofluoroscopy. Infant Behav Dev. 2010; 33:209–218. PMID: 20181397.
Article4. Williamson LR. Early feeding skills assessment in preterm infants [dissertation]. Lawrence: University of Kansas;2013.5. Thoyre SM, Shaker CS, Pridham KF. The early feeding skills assessment for preterm infants. Neonatal Netw. 2005; 24:7–16.
Article6. Langmore SE, Schatz K, Olson N. Endoscopic and videofluoroscopic evaluations of swallowing and aspiration. Ann Otol Rhinol Laryngol. 1991; 100:678–681. PMID: 1872520.
Article7. Mercado-Deane MG, Burton EM, Harlow SA, Glover AS, Deane DA, Guill MF, et al. Swallowing dysfunction in infants less than 1 year of age. Pediatr Radiol. 2001; 31:423–428. PMID: 11436889.
Article8. Browne JV, Ross ES. Eating as a neurodevelopmental process for high-risk newborns. Clin Perinatol. 2011; 38:731–743. PMID: 22107901.
Article9. Law-Morstatt L, Judd DM, Snyder P, Baier RJ, Dhanireddy R. Pacing as a treatment technique for transitional sucking patterns. J Perinatol. 2003; 23:483–488. PMID: 13679936.
Article10. Logemann JA. Evaluation and treatment of swallowing disorders. 2nd ed. San Diego: College Hill Press;1998. p. 168–180.11. Uhm KE, Yi SH, Chang HJ, Cheon HJ, Kwon JY. Videofluoroscopic swallowing study findings in full-term and preterm infants with Dysphagia. Ann Rehabil Med. 2013; 37:175–182. PMID: 23705111.
Article12. Ko MJ, Kang MJ, Ko KJ, Ki YO, Chang HJ, Kwon JY. Clinical usefulness of Schedule for Oral-Motor Assessment (SOMA) in children with dysphagia. Ann Rehabil Med. 2011; 35:477–484. PMID: 22506162.
Article13. Marofi M, Abedini F, Mohammadizadeh M, Talakoub S. Effect of palady and cup feeding on premature neonates' weight gain and reaching full oral feeding time interval. Iran J Nurs Midwifery Res. 2016; 21:202–206. PMID: 27095996.14. Rocha AD, Moreira ME, Pimenta HP, Ramos JR, Lucena SL. A randomized study of the efficacy of sensorymotor-oral stimulation and non-nutritive sucking in very low birthweight infant. Early Hum Dev. 2007; 83:385–388. PMID: 16979854.
Article15. Gewolb IH, Vice FL, Schwietzer-Kenney EL, Taciak VL, Bosma JF. Developmental patterns of rhythmic suck and swallow in preterm infants. Dev Med Child Neurol. 2001; 43:22–27. PMID: 11201418.
Article16. Lau C, Smith EO, Schanler RJ. Coordination of sucks-wallow and swallow respiration in preterm infants. Acta Paediatr. 2003; 92:721–727. PMID: 12856985.
Article17. Joan CA, Linda B. Pediatric swallowing and feeding. 2nd ed. Albany: Singular;2001. p. 355–376.18. Jeong JY, Wang KC, Bang MS. Introduction to cerebral palsy. Seoul: Koonja;2013. p. 209–213.19. Reilly S, Skuse D, Mathisen B, Wolke D. The object rating of oral-motor functions during feeding. Dysphagia. 1995; 10:117–191. PMID: 7600853.20. Skuse D, Stevenson J, Reilly S, Mathisen B. Schedule for oral-motor assessment (SOMA): methods of validation. Dysphagia. 1995; 10:192–202. PMID: 7614861.
Article21. Howe TH, Lin KC, Fu CP, Su CT, Hsieh CL. A review of psychometric properties of feeding assessment tools used in neonates. J Obstet Gynecol Neonatal Nurs. 2008; 37:338–349.
Article22. Braun MA, Palmer MM. A pilot study of oral-motor dysfunction in “at-risk” infants. Phys Occup Ther Pediatr. 1986; 5:13–25.
Article23. Philbin MK, Ross ES. The SOFFI Reference Guide: text, algorithms, and appendices: a manualized method for quality bottle-feedings. J Perinat Neonatal Nurs. 2011; 25:360–380. PMID: 22071621.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development of a Breast Feeding Adaptation Scale (BFAS)
- Clinical Validity of the Functional Dysphagia Scale Based on Videofluoroscopic Swallowing Study
- Development of a Premature Infant Pain Scale (PIPS)
- Development of a Dysphagia Screening Test for Preterm Infants (DST-PI)
- Developing the Mansoura Early Feeding Skills Assessment Scale for Preterm Infants