Clin Endosc.
2017 Jul;50(4):379-387. 10.5946/ce.2016.058.
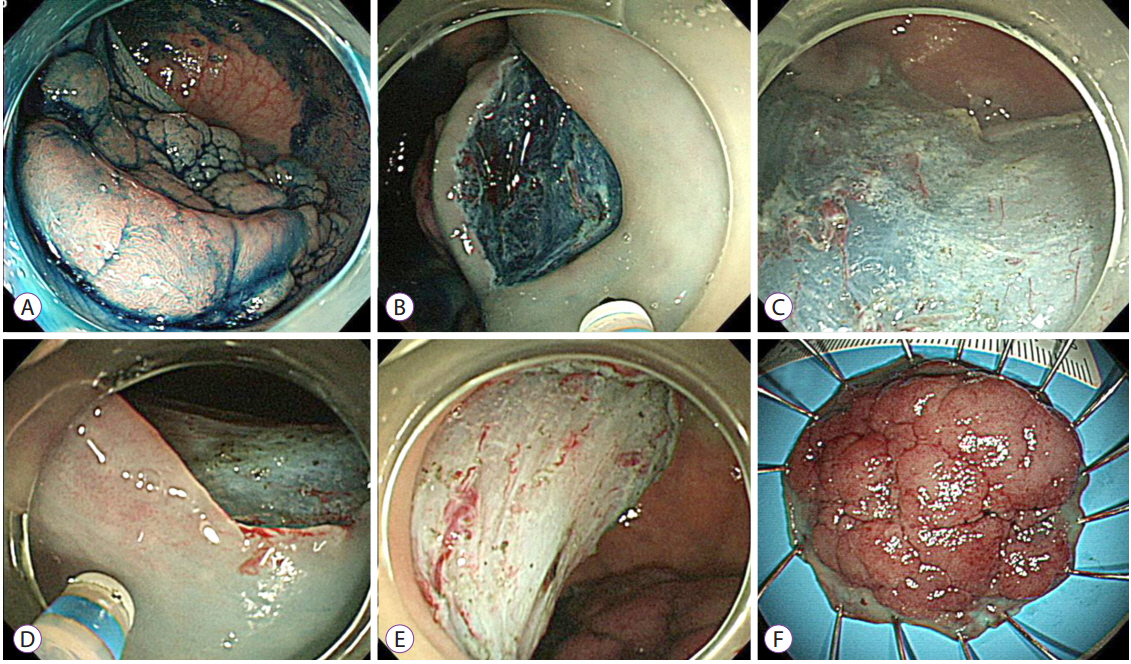
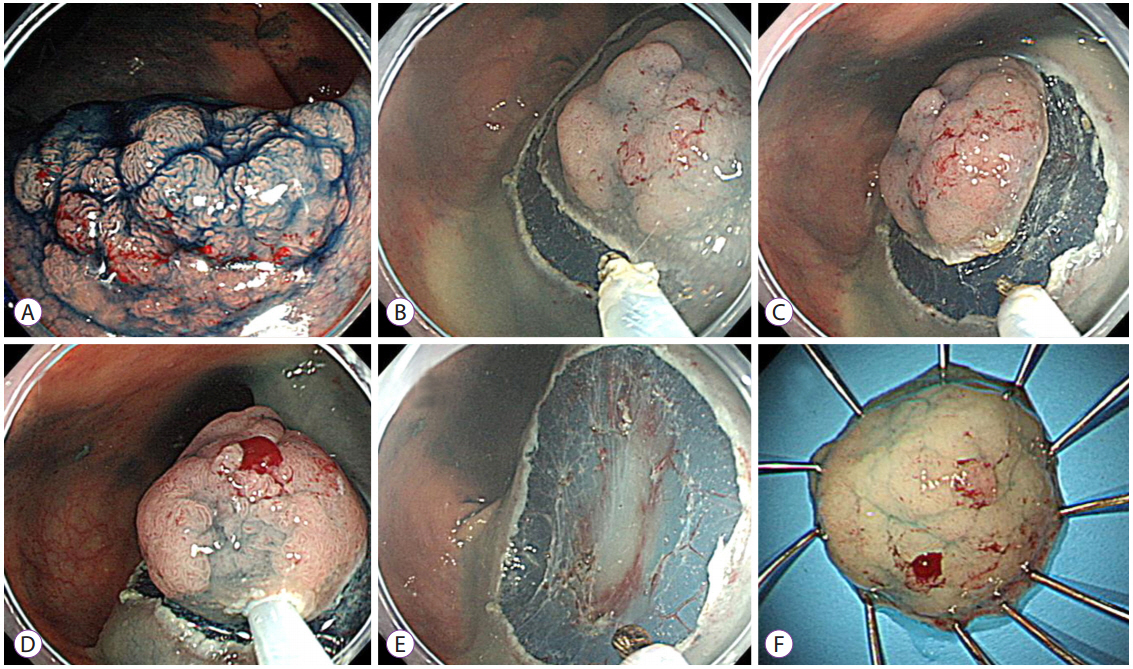
Endoscopic Mucosal Resection with Circumferential Mucosal Incision for Colorectal Neoplasms: Comparison with Endoscopic Submucosal Dissection and between Two Endoscopists with Different Experiences
- Affiliations
-
- 1Department of Gastroenterology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. dhyang@amc.seoul.kr
- 2Institute for Digestive Research, Soonchunhyang University College of Medicine, Seoul, Korea.
- 3Department of Gastroenterology and Hepatology, Stanford University School of Medicine, Stanford, Department of Gastroenterology, VA Palo Alto Health Care System, Palo Alto, CA, USA. shai_friedland@yahoo.com
- KMID: 2389244
- DOI: http://doi.org/10.5946/ce.2016.058
Abstract
- BACKGROUND/AIMS
Endoscopic mucosal resection with circumferential mucosal incision (CMI-EMR) may offer benefits comparable to those of endoscopic submucosal dissection (ESD), while requiring less technical proficiency than ESD.
METHODS
We retrospectively compared the outcomes of CMI-EMR (n=34) and size-matched ESD (n=102), which were performed by a Korean endoscopist for colorectal epithelial lesions of 20-35 mm. Procedural parameters of CMI-EMRs performed by an American ESD novice (n=30) were compared with those performed by the Korean endoscopist.
RESULTS
The lesion size was 22.3±3.9 mm and 22.9±2.4 mm in the CMI-EMR and size-matched ESD groups, respectively (p=0.730). The resection time was 12.7±7.0 minutes in the CMI-EMR group and 45.6±30.1 minutes in the ESD group (p<0.001). The en bloc resection rate was 94.1% in the CMI-EMR group and 100% in the ESD group (p=0.061). There were no differences in the en bloc resection and complication rates of CMI-EMRs between a Korean and an American endoscopist.
CONCLUSIONS
For the treatment of moderate-size colorectal lesions, CMI-EMR showed a trend toward lower en bloc resection rate, but required shorter procedure time than ESD. CMI-EMR outcomes were similar when performed by a Korean ESD expert and an American ESD novice.
Figure
Cited by 3 articles
-
Efficacy and Safety of Complete Endoscopic Resection of Colorectal Neoplasia Using a Stepwise Endoscopic Protocol with SOUTEN, a Novel Multifunctional Snare
Shinji Yoshii, Marina Kubo, Mio Matsumoto, Takefumi Kikuchi, Yasunari Takakuwa
Clin Endosc. 2020;53(2):206-212. doi: 10.5946/ce.2019.117.Pyogenic Liver Abscess Caused by Endoscopic Submucosal Dissection for Early Colon Cancer
Joon Seop Lee, Yong Hwan Kwon
Clin Endosc. 2019;52(6):620-623. doi: 10.5946/ce.2018.185.Filling the Technical Gap between Standard Endoscopic Mucosal Resection and Full Endoscopic Submucosal Dissection for 20–35 mm Sized Colorectal Neoplasms
Sung Noh Hong
Clin Endosc. 2017;50(4):313-315. doi: 10.5946/ce.2017.107.
Reference
-
1. Saito Y, Fukuzawa M, Matsuda T, et al. Clinical outcome of endoscopic submucosal dissection versus endoscopic mucosal resection of large colorectal tumors as determined by curative resection. Surg Endosc. 2010; 24:343–352.
Article2. Kobayashi N, Yoshitake N, Hirahara Y, et al. Matched case-control study comparing endoscopic submucosal dissection and endoscopic mucosal resection for colorectal tumors. J Gastroenterol Hepatol. 2012; 27:728–733.
Article3. Terasaki M, Tanaka S, Oka S, et al. Clinical outcomes of endoscopic submucosal dissection and endoscopic mucosal resection for laterally spreading tumors larger than 20 mm. J Gastroenterol Hepatol. 2012; 27:734–740.4. Saito Y, Uraoka T, Yamaguchi Y, et al. A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video). Gastrointest Endosc. 2010; 72:1217–1225.
Article5. Byeon JS, Yang DH, Kim KJ, et al. Endoscopic submucosal dissection with or without snaring for colorectal neoplasms. Gastrointest Endosc. 2011; 74:1075–1083.
Article6. Lee EJ, Lee JB, Choi YS, et al. Clinical risk factors for perforation during endoscopic submucosal dissection (ESD) for large-sized, nonpedunculated colorectal tumors. Surg Endosc. 2012; 26:1587–1594.
Article7. Hirao M, Masuda K, Asanuma T, et al. Endoscopic resection of early gastric cancer and other tumors with local injection of hypertonic saline-epinephrine. Gastrointest Endosc. 1988; 34:264–269.
Article8. Kim JJ, Lee JH, Jung HY, et al. EMR for early gastric cancer in Korea: a multicenter retrospective study. Gastrointest Endosc. 2007; 66:693–700.9. Cai S, Zhong Y, Zhou P, Xu J, Yao L. Re-evaluation of indications and outcomes of endoscopic excision procedures for colorectal tumors: a review. Gastroenterol Rep (Oxf). 2014; 2:27–36.
Article10. Min BH, Lee JH, Kim JJ, et al. Clinical outcomes of endoscopic submucosal dissection (ESD) for treating early gastric cancer: comparison with endoscopic mucosal resection after circumferential precutting (EMR-P). Dig Liver Dis. 2009; 41:201–209.
Article11. Huang J, Lu ZS, Yang YS, et al. Endoscopic mucosal resection with circumferential incision for treatment of rectal carcinoid tumours. World J Surg Oncol. 2014; 12:23.
Article12. Sakamoto T, Matsuda T, Nakajima T, Saito Y. Efficacy of endoscopic mucosal resection with circumferential incision for patients with large colorectal tumors. Clin Gastroenterol Hepatol. 2012; 10:22–26.
Article13. Lee EJ, Lee JB, Lee SH, Youk EG. Endoscopic treatment of large colorectal tumors: comparison of endoscopic mucosal resection, endoscopic mucosal resection-precutting, and endoscopic submucosal dissection. Surg Endosc. 2012; 26:2220–2230.
Article14. Hong YM, Kim HW, Park SB, Choi CW, Kang DH. Endoscopic mucosal resection with circumferential incision for the treatment of large sessile polyps and laterally spreading tumors of the colorectum. Clin Endosc. 2015; 48:52–58.
Article15. Yang DH, Jeong GH, Song Y, et al. The feasibility of performing colorectal endoscopic submucosal dissection without previous experience in performing gastric endoscopic submucosal dissection. Dig Dis Sci. 2015; 60:3431–3441.
Article16. Feitoza AB, Gostout CJ, Burgart LJ, Burkert A, Herman LJ, Rajan E. Hydroxypropyl methylcellulose: a better submucosal fluid cushion for endoscopic mucosal resection. Gastrointest Endosc. 2003; 57:41–47.
Article17. Hyun JJ, Chun HR, Chun HJ, et al. Comparison of the characteristics of submucosal injection solutions used in endoscopic mucosal resection. Scand J Gastroenterol. 2006; 41:488–492.18. Fasoulas K, Lazaraki G, Chatzimavroudis G, et al. Endoscopic mucosal resection of giant laterally spreading tumors with submucosal injection of hydroxyethyl starch: comparative study with normal saline solution. Surg Laparosc Endosc Percutan Tech. 2012; 22:272–278.19. Fujishiro M, Yahagi N, Nakamura M, et al. Successful outcomes of a novel endoscopic treatment for GI tumors: endoscopic submucosal dissection with a mixture of high-molecular-weight hyaluronic acid, glycerin, and sugar. Gastrointest Endosc. 2006; 63:243–249.
Article20. Toyonaga T, Man-I M, Morita Y, Azuma T. Endoscopic submucosal dissection (ESD) versus simplified/hybrid ESD. Gastrointest Endosc Clin N Am. 2014; 24:191–199.
Article21. Tanaka S, Kashida H, Saito Y, et al. JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc. 2015; 27:417–434.
Article22. Buchner AM, Guarner-Argente C, Ginsberg GG. Outcomes of EMR of defiant colorectal lesions directed to an endoscopy referral center. Gastrointest Endosc. 2012; 76:255–263.
Article23. Luigiano C, Consolo P, Scaffidi MG, et al. Endoscopic mucosal resection for large and giant sessile and flat colorectal polyps: a single-center experience with long-term follow-up. Endoscopy. 2009; 41:829–835.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- History and Development of Accessories for Endoscopic Submucosal Dissection
- Endoscopic Management of Gastric Subepithelial Tumor
- Endoscopic Submucosal Dissection for Gastric Tumors: Complete Resection Rate, Resection Time and Complications in Comparison with Endoscopic Mucosal Resection after Circumferential Mucosal Incision with a Needle Knife
- Debates on Colorectal Endoscopic Submucosal Dissection - Traction for Effective Dissection: Gravity Is Enough
- Tips and Tricks for Better Endoscopic Treatment of Colorectal Tumors: Usefulness of Cap and Band in Colorectal Endoscopic Mucosal Resection