Clin Endosc.
2017 Jul;50(4):366-371. 10.5946/ce.2016.155.
Health-Care Utilization and Complications of Endoscopic Esophageal Dilation in a National Population
- Affiliations
-
- 1Department of Internal Medicine, Einstein Medical Center, Philadelphia, PA, USA. goyalabh@einstein.edu
- 2University of Arkansas for Medical Sciences, Little Rock, AR, USA.
- 3Department of Gastroenterology, University of Nebraska Medical Center, Omaha, NE, USA.
- KMID: 2389242
- DOI: http://doi.org/10.5946/ce.2016.155
Abstract
- BACKGROUND/AIMS
Esophageal stricture is usually managed with outpatient endoscopic dilation. However, patients with food impaction or failure to thrive undergo inpatient dilation. Esophageal perforation is the most feared complication, and its risk in inpatient setting is unknown.
METHODS
We used National Inpatient Sample (NIS) database for 2007-2013. International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM) codes were used to identify patients with esophageal strictures. Logistic regression was used to assess association between hospital/patient characteristics and utilization of esophageal dilation.
RESULTS
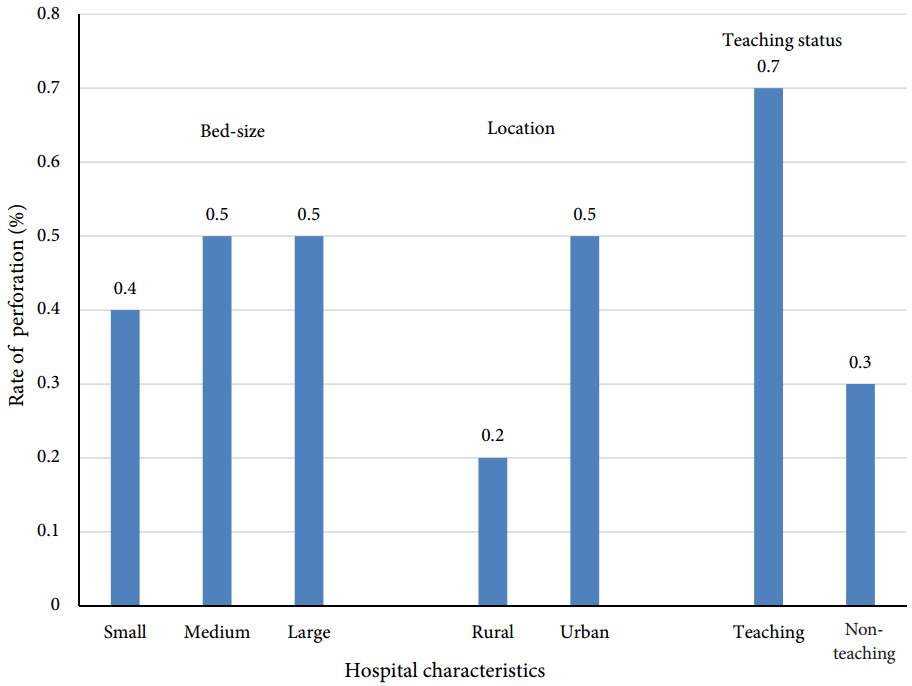
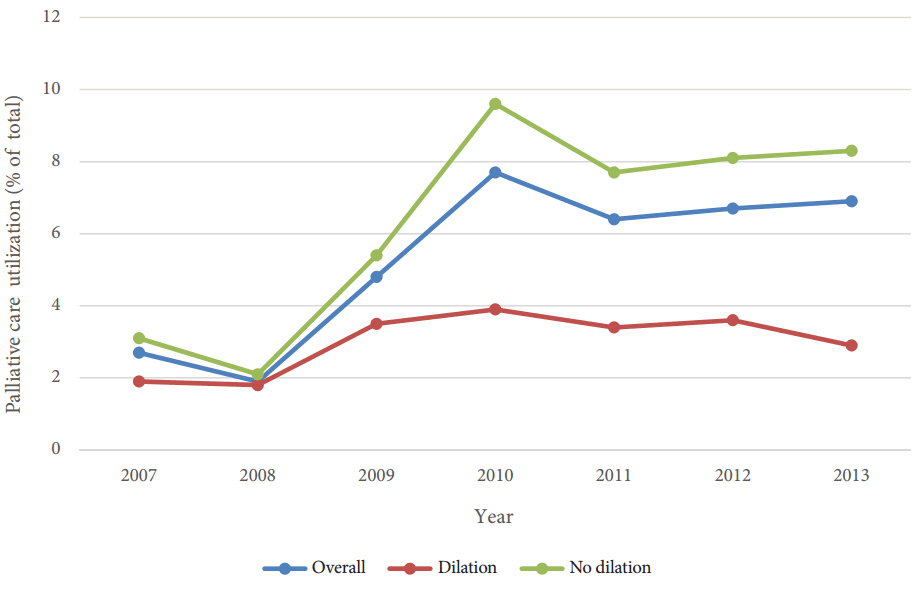
There were 591,187 hospitalizations involving esophageal stricture; 4.2% were malignant. Endoscopic dilation was performed in 28.7% cases. Dilation was more frequently utilized (odds ratio [OR], 1.36; p<0.001), had higher in-hospital mortality (3.1% vs. 1.4%, p<0.001), and resulted in longer hospital stays (5 days vs. 4 days, p=0.01), among cases of malignant strictures. Esophageal perforation was more common in the malignant group (0.9% vs. 0.5%, p=0.007). Patients with malignant compared to benign strictures undergoing dilation were more likely to require percutaneous endoscopic gastrostomy or jejunostomy (PEG/J) tube (14.1% vs. 4.5%, p<0.001). Palliative care services were utilized more frequently in malignant stricture cases not treated with dilation compared to those that were dilated.
CONCLUSIONS
Inpatient endoscopic dilation was utilized in 29% cases of esophageal stricture. Esophageal perforation, although infrequent, is more common in malignant strictures.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Safe and Proper Management of Esophageal Stricture Using Endoscopic Esophageal Dilation
Jae Jin Hwang
Clin Endosc. 2017;50(4):309-310. doi: 10.5946/ce.2017.100.
Reference
-
1. ASGE Standards of Practice Committee, Pasha SF, Acosta RD, et al. The role of endoscopy in the evaluation and management of dysphagia. Gastrointest Endosc. 2014; 79:191–201.
Article2. Richter JE. Peptic strictures of the esophagus. Gastroenterol Clin North Am. 1999; 28:875–891. vi.
Article3. Piotet E, Escher A, Monnier P. Esophageal and pharyngeal strictures: report on 1,862 endoscopic dilatations using the Savary-Gilliard technique. Eur Arch Otorhinolaryngol. 2008; 265:357–364.
Article4. Standards of Practice Committee, Egan JV, Baron TH, et al. Esophageal dilation. Gastrointest Endosc. 2006; 63:755–760.
Article5. Brinster CJ, Singhal S, Lee L, Marshall MB, Kaiser LR, Kucharczuk JC. Evolving options in the management of esophageal perforation. Ann Thorac Surg. 2004; 77:1475–1483.
Article6. AHRQ. NIS overview [Internet]. Rockville (MD): Healthcare cost and utilization project (HCUP);c2016. [updated 2016 Dec 14; cited 2016 Dec 15]. Available from: https://www.hcup-us.ahrq.gov/nisoverview.jsp.7. Zhang Y. Epidemiology of esophageal cancer. World J Gastroenterol. 2013; 19:5598–5606.
Article8. Shami VM. Endoscopic management of esophageal strictures. Gastroenterol Hepatol (N Y). 2014; 10:389–391.9. Fry LC, Mönkemüller K, Neumann H, Schulz HU, Malfertheiner P. Incidence, clinical management and outcomes of esophageal perforations after endoscopic dilatation. Z Gastroenterol. 2007; 45:1180–1184.
Article10. Hernandez LV, Jacobson JW, Harris MS. Comparison among the perforation rates of Maloney, balloon, and savary dilation of esophageal strictures. Gastrointest Endosc. 2000; 51(4 Pt 1):460–462.
Article11. Jethwa P, Lala A, Powell J, McConkey CC, Gillison EW, Spychal RT. A regional audit of iatrogenic perforation of tumours of the oesophagus and cardia. Aliment Pharmacol Ther. 2005; 21:479–484.
Article12. Pereira-Lima JC, Ramires RP, Zamin I Jr, Cassal AP, Marroni CA, Mattos AA. Endoscopic dilation of benign esophageal strictures: report on 1043 procedures. Am J Gastroenterol. 1999; 94:1497–1501.
Article13. Silvis SE, Nebel O, Rogers G, Sugawa C, Mandelstam P. Endoscopic complications. Results of the 1974 American society for gastrointestinal endoscopy survey. JAMA. 1976; 235:928–930.14. Riley SA, Attwood SE. Guidelines on the use of oesophageal dilatation in clinical practice. Gut. 2004; 53 Suppl 1:i1–i6.
Article15. Langdon DF. The rule of three in esophageal dilation. Gastrointest Endosc. 1997; 45:111.16. Hagel AF, Naegel A, Dauth W, et al. Perforation during esophageal dilatation: a 10-year experience. J Gastrointestin Liver Dis. 2013; 22:385–389.17. Mocanu A, Bârla R, Hoara P, Constantinoiu S. Endoscopic palliation of advanced esophageal cancer. J Med Life. 2015; 8:193–201.18. The American cancer society medical and editorial content team. Palliative therapy for cancer of the esophagus [Internet]. Atlanta (GA): American cancer society;c2014. [updated 2016 Feb 4; cited 2016 Dec 15]. Available from: https://www.cancer.org/cancer/esophagus-cancer/ treating/palliative-therapy.html.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Management of Dysphagia
- Benign Esophageal Stricture
- Accidentally Confirmed Relapse of Plummer-Vinson Syndrome during Esophageal Foreign Body Evaluation
- Stent Flange-Induced Esophageal Stricture Treated with an Oral Steroid
- Safe and Proper Management of Esophageal Stricture Using Endoscopic Esophageal Dilation