Korean Circ J.
2015 May;45(3):225-233. 10.4070/kcj.2015.45.3.225.
Additive Beneficial Effects of Valsartan Combined with Rosuvastatin in the Treatment of Hypercholesterolemic Hypertensive Patients
- Affiliations
-
- 1Division of Cardiology and Cardiovascular Research Institute, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. jangys1212@yuhs.ac
- 2Division of Cardiology, Department of Internal Medicine, Daedong Hospital, Busan, Korea.
- 3Division of Cardiology, Cardiovascular Center, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea.
- 4Division of Cardiology, Department of Internal Medicine, Kyung Hee University Medical Center, Seoul, Korea.
- 5Department of Cardiology, Heart Research Center of Chonnam National University Hospital, Gwangju, Korea.
- 6Department of Cardiology, Soon Chun Hyang University Bucheon Hospital, Bucheon, Korea.
- 7Department of Cardiology, Gachon University Gil Medical Center, Incheon, Korea.
- 8Division of Cardiology, Dankook University College of Medicine, Cheonan, Korea.
- 9Division of Cardiology, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea.
- 10Division of Cardiology, Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 11Division of Cardiology, Department of Internal Medicine, Konyang University Hospital, Daejeon, Korea.
- 12Department of Cardiology, Ajou University Medical Center, Suwon, Korea.
- 13Division of Cardiology, Pusan National University Hospital, Busan, Korea.
- 14Division of Cardiology, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 15Division of Cardiology, Department of Internal Medicine, Gyeongsang National University Hospital and Gyeongsang National University School of Medicine, Jinju, Korea.
- 16Department of Cardiology, Myongji Hospital Cardiovascular Center, Goyang, Korea.
- 17Division of Cardiology, Department of Internal Medicine, Yeungnam University Hospital, Daegu, Korea.
- 18Division of Cardiology, Department of Internal Medicine, SMG-SNU Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea.
- 19Division of Cardiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 20Division of Cardiology, Department of Internal Medicine, Ewha Womans University Mokdong Hospital, Seoul, Korea.
- 21Department of Cardiology, Pusan National University Yangsan Hospital, Yangsan, Korea.
- 22Division of Cardiology, Department of Internal Medicine, Inje University Ilsan Paik Hospital, Goyang, Korea.
- 23Division of Cardiology, Department of Internal Medicine, Kosin University Gospel Hospital, Busan, Korea.
- 24Clinical Development Department, LG Life Sciences Ltd., Seoul, Korea.
- KMID: 2389130
- DOI: http://doi.org/10.4070/kcj.2015.45.3.225
Abstract
- BACKGROUND AND OBJECTIVES
We compared the efficacy and safety of valsartan and rosuvastatin combination therapy with each treatment alone in hypercholesterolemic hypertensive patients.
SUBJECTS AND METHODS
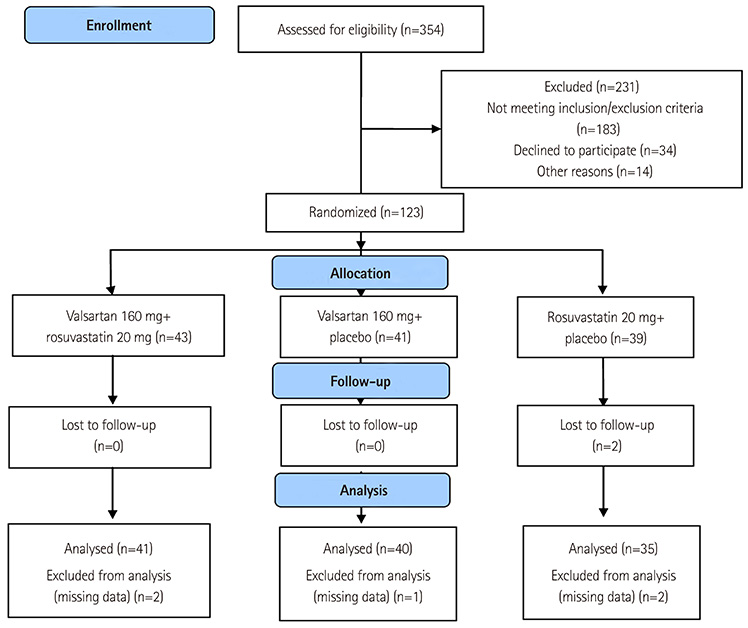
Patients who met inclusion criteria were randomized to receive 1 of the following 2-month drug regimens: valsartan 160 mg plus rosuvastatin 20 mg, valsartan 160 mg plus placebo, or rosuvastatin 20 mg plus placebo. The primary efficacy variables were change in sitting diastolic blood pressure (sitDBP) and sitting systolic blood pressure (sitSBP), and percentage change in low-density lipoprotein-cholesterol (LDL-C) in the combination, valsartan, and rosuvastatin groups. Adverse events (AEs) during the study were analyzed.
RESULTS
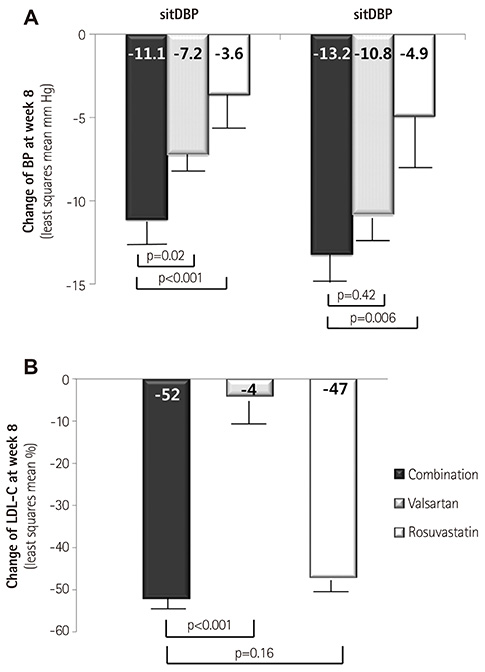
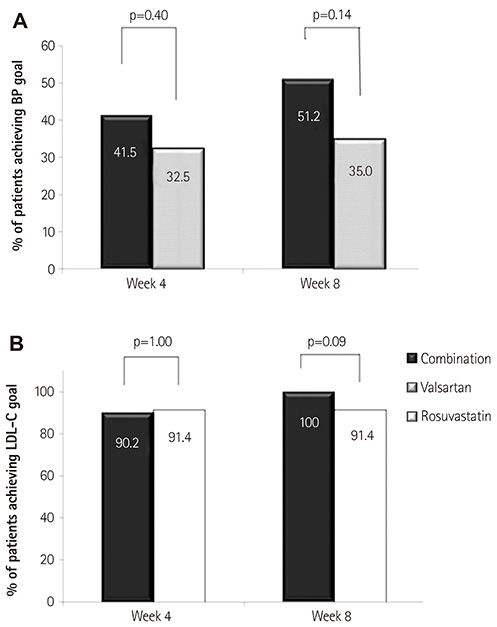
A total of 354 patients were screened and 123 of them were finally randomized. Changes of sitDBP by least squares mean (LSM) were -11.1, -7.2, and -3.6 mm Hg, respectively, and was greater in the combination, as compared to both valsartan (p=0.02) and rosuvastatin (p<0.001). Changes of sitSBP by LSM were -13.2, -10.8, and -4.9 mm Hg, and was greater in the combination, as compared to rosuvastatin (p=0.006) and not valsartan (p=0.42). Percentage changes of LDL-C by LSM were -52, -4, and -47% in each group, and was greater in the combination, as compared to valsartan (p<0.001), similar to rosuvastatin (p=0.16). Most AEs were mild and resolved by the end of the study.
CONCLUSION
Combination treatment with valsartan and rosuvastatin exhibited an additive blood pressure-lowering effect with acceptable tolerability, as compared to valsartan monotherapy. Its lipid lowering effect was similar to rosuvatatin monotherapy.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Fixed-dose combination therapy for cardiovascular prevention
Sang-Hak Lee
J Korean Med Assoc. 2016;59(11):883-887. doi: 10.5124/jkma.2016.59.11.883.Blood pressure lowering effect of statin drugs with an application to rosuvastatin
Young-A Heo, Mijeong Son, Kyungsoo Park
Transl Clin Pharmacol. 2016;24(3):132-136. doi: 10.12793/tcp.2016.24.3.132.
Reference
-
1. Kannel WB. Blood pressure as a cardiovascular risk factor: prevention and treatment. JAMA. 1996; 275:1571–1576.2. Thomas F, Bean K, Guize L, Quentzel S, Argyriadis P, Benetos A. Combined effects of systolic blood pressure and serum cholesterol on cardiovascular mortality in young (<55 years) men and women. Eur Heart J. 2002; 23:528–535.3. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014; 311:507–520.4. Nickenig G, Harrison DG. The AT(1)-type angiotensin receptor in oxidative stress and atherogenesis: Part II: AT(1) receptor regulation. Circulation. 2002; 105:530–536.5. Keidar S, Kaplan M, Shapira C, Brook JG, Aviram M. Low density lipoprotein isolated from patients with essential hypertension exhibits increased propensity for oxidation and enhanced uptake by macrophages: a possible role for angiotensin II. Atherosclerosis. 1994; 107:71–84.6. Pool JL, Glazer R, Chiang YT, Gatlin M. Dose-response efficacy of valsartan, a new angiotensin II receptor blocker. J Hum Hypertens. 1999; 13:275–281.7. Pfeffer MA, McMurray JJ, Velazquez EJ, et al. Valsartan, captopril, or both in myocardial infarction complicated by heart failure, left ventricular dysfunction, or both. N Engl J Med. 2003; 349:1893–1906.8. Julius S, Kjeldsen SE, Weber M, et al. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trial. Lancet. 2004; 363:2022–2031.9. Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014; 63:2889–2934.10. White CM. A review of the pharmacologic and pharmacokinetic aspects of rosuvastatin. J Clin Pharmacol. 2002; 42:963–970.11. Borghi C, Prandin MG, Costa FV, Bacchelli S, Degli Esposti D, Ambrosioni E. Use of statins and blood pressure control in treated hypertensive patients with hypercholesterolemia. J Cardiovasc Pharmacol. 2000; 35:549–555.12. Glorioso N, Troffa C, Filigheddu F, et al. Effect of the HMG-CoA reductase inhibitors on blood pressure in patients with essential hypertension and primary hypercholesterolemia. Hypertension. 1999; 34:1281–1286.13. Sposito AC, Mansur AP, Coelho OR, et al. Additional reduction in blood pressure after cholesterol-lowering treatment by statins (lovastatin or pravastatin) in hypercholesterolemic patients using angiotensin-converting enzyme inhibitors (enalapril or lisinopril). Am J Cardiol. 1999; 83:1497–1499.14. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA. 2001; 285:2486–2497.15. Cifkova R, Erdine S, Fagard R, et al. Practice guidelines for primary care physicians: 2003 ESH/ESC hypertension guidelines. J Hypertens. 2003; 21:1779–1786.16. Philipp T, Smith TR, Glazer R, et al. Two multicenter, 8-week, randomized, double-blind, placebo-controlled, parallel-group studies evaluating the efficacy and tolerability of amlodipine and valsartan in combination and as monotherapy in adult patients with mild to moderate essential hypertension. Clin Ther. 2007; 29:563–580.17. Avis HJ, Hutten BA, Gagné C, et al. Efficacy and safety of rosuvastatin therapy for children with familial hypercholesterolemia. J Am Coll Cardiol. 2010; 55:1121–1126.18. Wilson TW, Alonso-Galicia M, Roman RJ. Effects of lipid-lowering agents in the Dahl salt-sensitive rat. Hypertension. 1998; 31:225–231.19. Jiang J, Roman RJ. Lovastatin prevents development of hypertension in spontaneously hypertensive rats. Hypertension. 1997; 30:968–974.20. Nazzaro P, Manzari M, Merlo M, et al. Distinct and combined vascular effects of ACE blockade and HMG-CoA reductase inhibition in hypertensive subjects. Hypertension. 1999; 33:719–725.21. Borghi C, Dormi A, D'Addato S, et al. Trends in blood pressure control and antihypertensive treatment in clinical practice: the Brisighella Heart Study. J Hypertens. 2004; 22:1707–1716.22. Rajagopalan S, Zannad F, Radauceanu A, et al. Effects of valsartan alone versus valsartan/simvastatin combination on ambulatory blood pressure, C-reactive protein, lipoproteins, and monocyte chemoattractant protein-1 in patients with hyperlipidemia and hypertension. Am J Cardiol. 2007; 100:222–226.23. O'Driscoll G, Green D, Taylor RR. Simvastatin, an HMG-coenzyme A reductase inhibitor, improves endothelial function within 1 month. Circulation. 1997; 95:1126–1131.24. Egede R, Jensen LO, Hansen HS, et al. Effect of intensive lipid-lowering treatment compared to moderate lipid-lowering treatment with rosuvastatin on endothelial function in high risk patients. Int J Cardiol. 2012; 158:376–379.25. Lewis TV, Cooper BA, Dart AM, Chin-Dusting JP. Responses to endothelium-dependent agonists in subcutaneous arteries excised from hypercholesterolaemic men. Br J Pharmacol. 1998; 124:222–228.26. Kaesemeyer WH, Caldwell RB, Huang J, Caldwell RW. Pravastatin sodium activates endothelial nitric oxide synthase independent of its cholesterol-lowering actions. J Am Coll Cardiol. 1999; 33:234–241.27. Straznicky NE, Howes LG, Lam W, Louis WJ. Effects of pravastatin on cardiovascular reactivity to norepinephrine and angiotensin II in patients with hypercholesterolemia and systemic hypertension. Am J Cardiol. 1995; 75:582–586.28. Savić V, Eržen B, Janić M, et al. Improvement of arterial wall characteristics by the low-dose fluvastatin and valsartan combination in type 1 diabetes mellitus patients. Diab Vasc Dis Res. 2013; 10:420–425.29. Koh KK, Quon MJ, Han SH, et al. Additive beneficial effects of losartan combined with simvastatin in the treatment of hypercholesterolemic, hypertensive patients. Circulation. 2004; 110:3687–3692.30. Roberts C, Torgerson DJ. Understanding controlled trials: baseline imbalance in randomized controlled trials. BMJ. 1999; 319:185.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum to: Additive Beneficial Effects of Valsartan Combined with Rosuvastatin in the Treatment of Hypercholesterolemic Hypertensive Patients
- Rosuvastatin-induced Generalized Drug Eruption
- Addition of Amlodipine or Valsartan for Improvement of Diastolic Dysfunction Associated with Hypertension
- Effect of Rosuvastatin on Coronary Flow Reserve in Hypertensive Patients at Cardiovascular Risk
- Letter: Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J 2019;43:582–9)